INTRODUCTION
Pancreatic panniculitis, also called subcutaneous fat necrosis, is a rare entity associated with pancreatic diseases. Its pathogenesis is still not well understood, but the release of pancreatic enzymes in the setting of pancreatic injury may play an important role. Clinically, patients most often present with painful skin nodules that spontaneously ulcerate and exude an oily, sterile, brown substance that results from liquefaction necrosis of adipocytes. It is important to be alert, because although their histological findings are characteristic, the clinical features of other panniculitis are similar.
Since its first description by Chiari in 1883, there have been reported few cases in the literature.
We described here a case of a patient with a history of chronic idiopathic pancreatitis, who developed a pancreatic panniculitis
CASE REPORT
A 53-year-old woman was admitted to the hospital with a 1-month history of asthenia, loss of appetite and painful erythematous-violaceous nodules on the extremities, as well as swelling of the knees and ankles, without heat or erythema. No fever was documented. Otherwise, the results of a review of the systems were normal. And she had no significant medication history changes recently.
At physical examination she looked well and was afebrile. No one of the nodules were ulcerated or were dreaining oily fluid, but she referred occasionally spontaneous yellowish liquid by some of them.
Her medical history include idiopathic chronic pancreatitis diagnosed over 15 years ago with several episodes of exacerbation and complications mainly in form of pancreatic cysts operated on several occasions; in control in our hospital, with clinical stability in recent months.
In the presence of painful subcutaneous nodules we considered the following diagnostic hypotheses: erythema nodosum, erythema induratum Bazin, SLE, sarcoidosis, cutaneous metastases, alpha-1-antitrypsin deficiency, polyarteritis nodosa, panniculitis-like subcutaneous lymphomas and infectious and traumatic origin. With the help of diagnostic tests that we report below and taking into account the medical history of the patient and the clinical and epidemiological manifestations, we could establish the diagnosis of pancreatic panniculitis origin.
Laboratory tests showed significant elevation serum amylase and lipase, a hemoglobin level of 8.3 with normal mean corpuscular volume, a white blood cell count of 3.68×109/L without eosinophilia and elevated acute reactant phase. The liver profile showed mild elevated serum transaminases, as usual in our patient for years. The remaining parameters, including renal function, inmunology, Mantoux, alpha-1-antitrypsin, angiotensin-converting enzyme or tumor marker, were within the normal range. Serologies as Mycoplasma, Yersinia, Chlamydia or Treponema were negatives. And blood cultures and nodular material cultures were also negatives.
The chest radiograph was normal and abdominal CT scan revealed the persistence of old scars in pancreas without evidence of exacerbation at the time.
Suspecting skin involvement in the context of her long pancreatic disease, a nodule biopsy was done to confirm the clinical diagnosis of panniculitis. Skin histopathlogy was pathognomonic: lobular panniculitis without vasculitis, with focal necrosis in adipocytes associated with ´ghost-like cells´ with microcalcifications inside and without vasculitis. Her study was completed by performing bone gammagraphy and bone marrow biopsy without evidence of extension or involvement of the fatty tissues; that fact have substantially poor prognosis. Symptomatic treatment was started with analgesics, rest and elevation of the extremities. The most of the skin lesions resolved spontaneuosly after 10 days and pancreatic enzymes returned to normal.
DISCUSSION
The subcutaneous fat necrosis is a rare type of panniculitis that appears only in 2-3% of all patients with pancreatic diseases, being in 40% of cases the first manifestation of them1. It is associated with acute or chronic pancreatitis and pancreatic carcinoma, usually acinar type, which is the best preserved their secretory capacity1,2. However, there are cases described after abdominal trauma, pancreatic pseudocyst, pancreas divisum, pancreatic vascular fistulas or after taking drugs such as oral contraceptives, cyclosporine or thiazides3. Most cases reported in the literature appear between the 4th and 6th decade of life, predominantly in males, attributed to increased consumption of alcohol4.
The pathogenesis is still unknown, but it is assumed the release of pancreatic enzymes, such as amylase, trypsin, lipase, chymotrypsin and elastase, may play a role. This is supported by the finding of these enzymes in the areas of subcutaneous fat necrosis and also anti-lipase monoclonal antibodies within the necrotic tissue1,4,5,6. There are probably other unknown factors required for the development of pancreatic panniculitis, because pancreatic disease is much more common than pancreatic panniculitis. Furthermore, in vitro studies did not demonstrate pancreatic panniculitis when normal human subcutaneous fat was incubated with human serum with high levels of pancreatic lipase and amylase, and some cases have been described with normal levels of pancreatic enzymes7,8. Another hypothesis is that these patients are unable to degrade pancreatic enzymes, probably due to inherited enzyme deficiencies such as alpha 1-antitrypsin5,9. This diversity of views makes the pathogenesis still controversial and need further studies.
Clinically, patients with panniculitis pancreatics most often present with subcutaneous nodules, erythematous-violaceous, usually painful and located in the tibial region and around the knees and ankles. Other locations as abdomen, chest, upper extremities and even the scalp, are also described10. These nodules may evolve to fluctuation and spontaneously ulcerate and drean an oily material by liquefaction of adipocytes. With the resolution of the process, the nodules are replaced by a pigmented macula scar (Fig 1), sometimes with atrophic surface4. Although the nodules often persist in the case of pancreatic carcinoma. The skin manifestations can precede, occur concurrently with or follow the pancreatic pathology1,5,11. In these cases the average interval between the cutaneous findings and the discovery of abdominal disease is 3-4 months11. More generalized cases also present with arthritis due to periarticular fat necrosis, not correlated with primary sinovitys, and serositis also as pleural effusion, pericardial effusion or ascites1,9. Fat necrosis may also affect the intramedullary bone fat, liver fat, intestinal fat and even central system nervous4. And it is believed that these features is associated with a poor prognosis.
Histological findings are very characteristic, therefore the biopsy of the skin lesions is the greater value test; as well, the clinical appearance of pancreatic panniculitis is nonspecific and it mimics other paniculitis (infectous, panarteritis or erythema nodosum). The main histopathologic feature is a mostly lobular panniculitis without vasculitis, with intense necrosis of adypocites (Fig 2)1,4,7. These necrotic adipocytes with no nuclei, thick wall and finely granular and basophilic material in the cytoplasm because of calcification are known as ghost cells. In older lesions, fat necrosis and calcified ghost adipocytes are less evident and fibrosis or lipoatrophy are seen.
Blood tests often demonstrate leukocytosis with eosinophilia, anemia and elevated serum amylase and/or lipase. In cases of normal serum amylase can be determined levels or clearance of amylase/creatinine in urine4.
Treatment is largely supportive and directed at the underlying pancreatic disorder5,9,12. The somatostatin analogue octeotride, corticosteroid and immunosupresive therapy could effectively not control the symptoms13. In patients with pancreatic carcinoma, the resection of pancreatic tumor should be performed as soon as possible, and if this is not successful, then treatment with combination chemotherapeutics may be administered.
The evolution and prognosis depend on the underlying disease and, ultimately, the extent of fat necrosis to other structures, more frequent in cases associated with pancreatic neoplasia14. Pancreatic panniculitis has a high mortality rate unless the underlying pancreatic abnormality is reversed.
In conclusion, we believe it is important to recognize these skin lesions because they may be an early marker of pancreatic disease, even in abscense of abdominal symptoms. Monitoring of these patients with laboratory and imaging test, is essential because the skin involvement may occur up to 15 weeks before the pancreatic dissorder. We must also remember that if the skin lesions are recurrent underlying disease is more likely to be a tumor.
Figura I

Lesão cutânea
Figura II
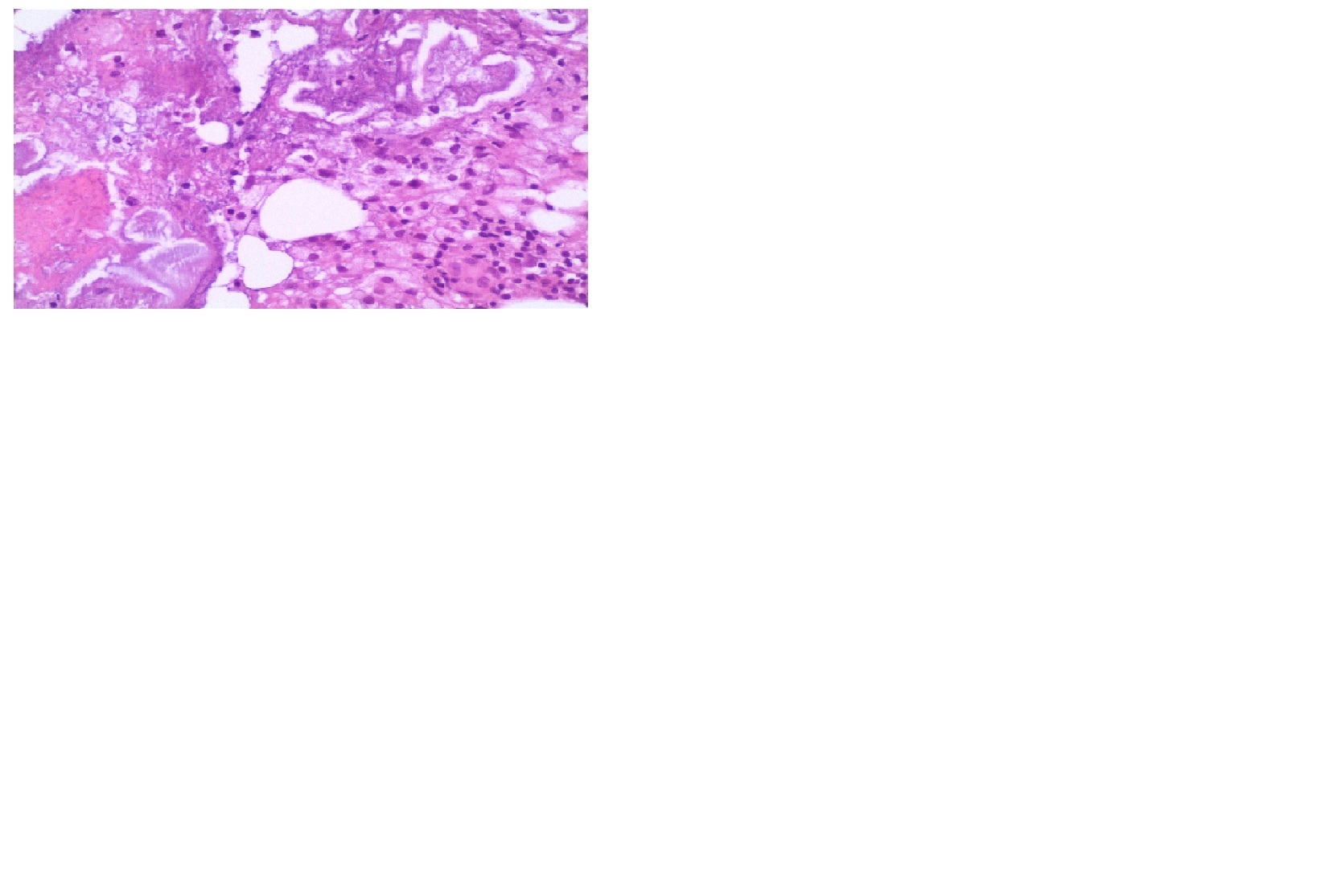
Visão ao microscopio
BIBLIOGRAFIA
Marsh RW, Hagler KT, Carag HR, Flowers FP. Pancreatic panniculitis. Eur J Surg Oncol. 2005;31:1213-5.
Poelman SM, Nguyen K. Pancreatic panniculitis associated with acinar cell pancreatic carcinoma. J Cutan Med Surg. 2008;12:38-42.
Detflets RL. Drug induced pancreatitis presenting as subcutaneous fat necrosis. J Am Acad Dermatol 1985;13:30-57.
Segurado Rodríguez A, Guerra Tapia A, Jaén Olasolo P, Cuevas Santos J. Paniculitis pancreática: estudio de 12 casos y valoración comparativa de sus caracteres epidemiológicos, clínicos, histopatológicos y terapéuticos. Actas Dermosifiliogr 1999; 90: 227-234.
Lee WS, Kim MY, Kim SW, Paik CN, Kim HO, Park YM. Fatal pancreatic panniculitis associated with acute pancreatitis: a case report. J Korean Med Sci. 2007;22:914-7
Wilson AA, Askari AD, Neiderhiser DH. Pancreatitis with arthropaty and subcutaneous fat necrosis: evidence for the pathogenicity of lipolytic enzimes. Arth Rheum 1983;26:121-6.
Dhawan SS, Jiménez Acosta F, Poppiti RJ, Barkim JS. Subcutaneous fat necrosis associated with pancreatitis: histochemical and electron microscopic findings. Am J Gastroenterol 1990;85:1025-8.
Requena L, Sánchez-Yus E. Panniculitis. Part II. Mostly lobular panniculitis. J Am Acad Dermatol. 2001;45:3253-61.
Farrant P, Abu-Nab Z, Hextall J. Tender erythematous nodules on the lower limb. Clin Exp Dermatol. 2009;34:549-51.
Potts DE, Mass MF, Iseman MD. Syndrome of pancreatic disease, subcutaneous fat necrosis and polyserositis: Case report and review of literature. Am J Med 1975;58:417-23.
Dahl PR, Su WP, Cullimore KC, Dicken CH. Pancreatic panniculitis. J Am Acad Dermatol. 1995;33:413-7.
Laureano A, Mestre T, Cardoso J. Pancreatic paniculitis, a cutaneous manifestation of acute pancreatitis. J Dermatol Case Rep. Mar 31, 2014; 8(1): 35-37.
Beltraminelli HS, Buechner SA, Häusermann P. Pancreatic panniculitis in a patient with an acinar cell cystadenocarcinoma of the pancreas. Dermatology. 2004;208:265-67.
Valle A. Gareis MC, Garritano MV, Russo JP, Chiavassa AM et al. Paniculitis pancreática. Arch. Argent. Dermatol. 2008;58:11-13.

