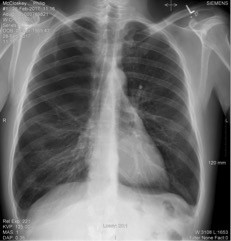
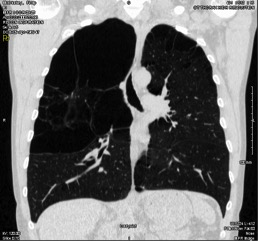
Vanishing lung syndrome is characterized by giant bullous emphysema presentation and is associated with significant morbidity and mortality. We are presenting a clinical case of a patient, male, 47 years old, carpenter by occupation. The patient was referred to us on 28/02/2017 for Shortness of Breath (SOB), functional class II (NYHA), worsening progressively since the past few months, with cough and whitish phlegm. No fever, night sweating or chills and no loss of weight. He was a chronic smoker with no other significant cardiovascular risk factors. Past history of right knee replacement some years ago and family history of emphysema. On admission, the patient was not in respiratory distress at rest and not cyanotic. Blood Pressure – 134/84 mmHg; Heart Rate – 66/min; Peripheral capillary oxygen saturation – 98% (Room Air); Respiratory Rate – 19/min; the breath sounds were diminished on the right upper half chest. Hgb - 14,8 g/dl; White Cell Count – 5,9x103; Platelet Count – 250x103; (mmol/l) Sodium - 138; Potassium - 4.4; Urea - 4.0; Creatinine – 64; ALT – 17; Gamma GT – 25; CRP - 1.5; Alpha 1 Antitrypsin - 1,5 (N: 0,9 – 2,0). The XR Chest (28/02/2017) showed a marked bullous emphysematous change noted, in particular, in the right apex, with no active lung lesion (Fig1). The CT-Thorax (23/03/2017) showed a marked paraseptal emphysematous change in the upper lobes. The changes were greater in the right upper lobe, where there were a large bulla measuring 12 cm or greater in size (Fig2). The Pulmonary Function Tests were done on 03/05/2017 and were reported as severe obstruction with incomplete reversibility and moderate impaired gas transfer. Vanishing lung syndrome (VLS) is a rare radiological syndrome that on XR Chest the lungs looks to be disappearing1. It is more common in young male smokers2and can be presented with a spontaneous pneumothorax and a bronchopleural fistula. In the chest XR Chest, the giant bullae can be misdiagnosed as a pneumothorax3. It remains unknown if some genetic inheritance is associated with the disease. It have been reported some cases of autosomal dominant and recessive inheritance4. It have also been reported raised Anti-dsDNA and anti-Ro/SSA and restrictive lung function5. Some patients with VLS and pneumothorax, has electrical alternation on ECG6.
Figura I
Figura II
BIBLIOGRAFIA
1 - J Assoc Physicians India.2014 Dec;62(12):51-3. A Rare Case ofVanishingLungSyndrome. Vij AS,James R,Singh A,Dhaliwal AS,Chhabra A,Vij KK.
2 - Ann Thorac Surg.2017 Mar;103(3):e277-e279. doi: 10.1016/j.athoracsur.2016.09.009. Intrabronchial Pneumonectomy forVanishingLungSyndrome: First Reported Case. Ballay N1,Soder B1,Smith J1,Miller A2,Headrick JR Jr1.
3 - Proc (Bayl Univ Med Cent).2016 Oct;29(4):399-401. Vanishing lung syndrome. Im Y1,Farooqi S1,Mora A Jr1.
4 - Mol Med Rep.2015 Jan;11(1):567-70. doi: 10.3892/mmr.2014.2673. Epub 2014 Oct 16. Vanishinglungsyndromein one family: five cases with a 20-year follow-up. Gao X1,Wang H2,Gou K3,Huang B1,Xia D1,Wu X1,Wei M1,Zheng S1,Ma S1,He J1.
5 - Laeknabladid.2017 Mai;102(5):237-240. doi: 10.17992/lbl.2017.05.137. [Vanishinglungs - a case report]. Thordardottir TH,Geirsson AJ,Hansdottir S.
6 - BMJ Case Rep.2015 Jan 23;2015. pii: bcr2014207498. doi: 10.1136/bcr-2014-207498. ECG phasic voltage changes associated with spontaneous pneumothorax in a patient with vanishing lung syndrome.Fei J1,Marill KA1.