Aortic dissection is defined as disruption of the medial layer provoked by intramural bleeding, resulting in separation of the aortic wall layers 1.
A 41-year-old man, with uncontrolled arterial hypertension was referred to the emergency department for retrosternal pain with a 10-hour course. The pain had interscapular irradiation, and was accompanied by profuse sweating. The physical examination showed a differential blood pressure of upper limbs (left 100/70 mmHg, right 165/83 mmHg); absence of left radial and brachial pulses and a holodiastolic aortic murmur.
Electrocardiogram revealed sinus rhythm 60/bpm plus left ventricular hypertrophy. A pocket size transthoracic echocardiogram (VSCAN®) was performed, showing a 63 mm ascending aorta aneurysm with an intimal flap. The dissection triggered the aortic arch, the descending aorta, and the brachiocephalic trunk. The aortic valve was tricuspid, with severe aortic insufficiency, due to dilation of the aortic root. CT angiography confirmed a type A Stanford aortic dissection, originating from the anterolateral ascending aorta wall. The dissection expanded to the abdominal aorta; to the 3 supra-aortic branches, and to the femoral arteries.
Labetalol perfusion was started and the patient was referred for emergent cardiac surgery. A Bentall surgical procedure was performed: i) a vascular prosthesis was inserted at the ascending aorta; ii) reimplantation of the coronary arteries and iii) replacement of the aortic valve with a mechanical prosthesis.
In current emergency practice, focused cardiac ultrasound has become a fundamental tool to expedite the diagnostic evaluation and to initiate emergent treatment2-3. Nevertheless, the focused imaging findings should always be integrated on the clinical probability assessment 4. In the context of a suspected acute aortic syndrome, further imaging or diagnostic studies may be considered when facing a normal or non-diagnostic VSCAN5-6.
Pocket size echocardiography education and training is of utmost importance for emergency physicians to optimize patient care.
Acknowledgments: I thank Rogério Teixeira MD, PhD for his contribution to the development of the image in clinical medicine and for commenting on early outlines for this image. I also thank for his involvement, comments and suggestions.
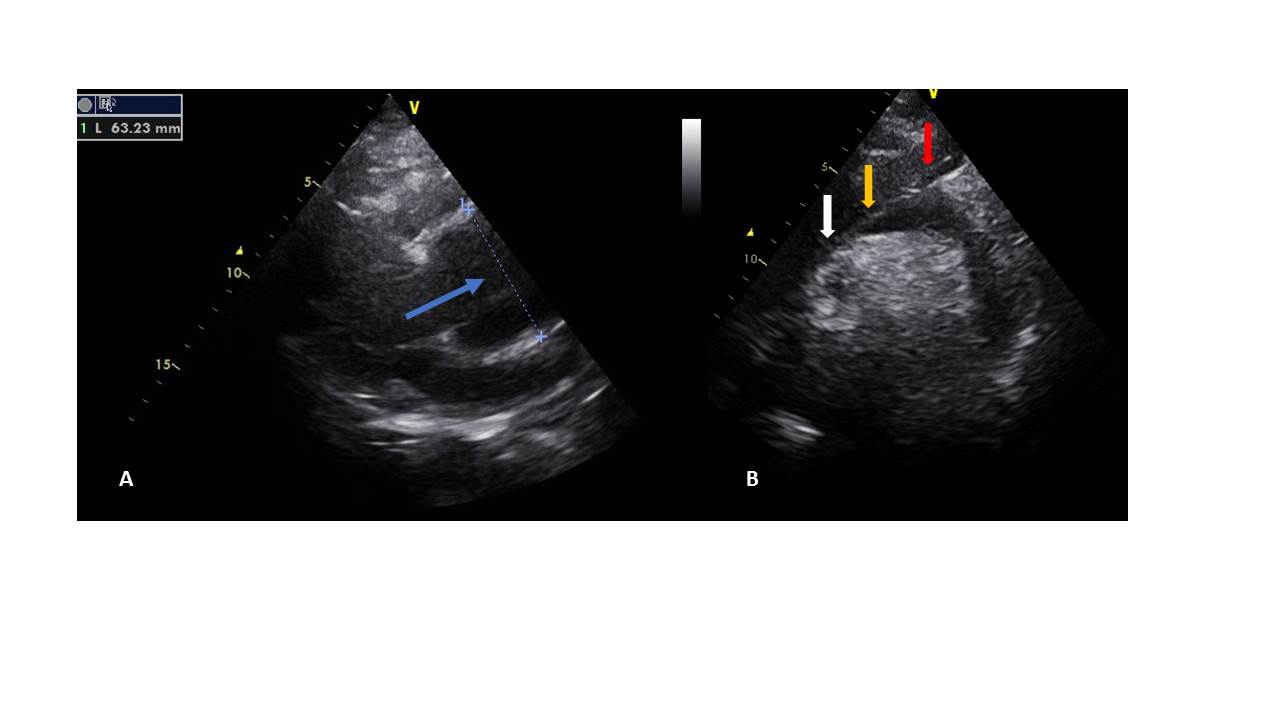
Figura I
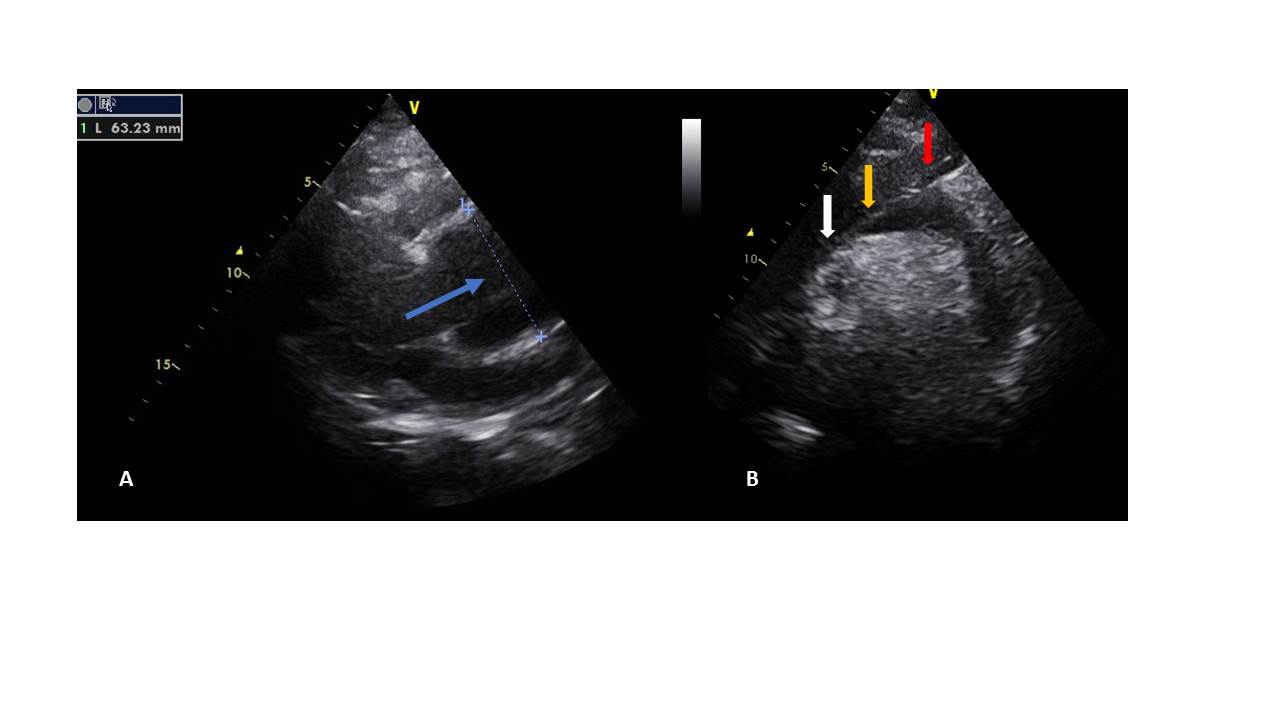
Panel A: paraesternal long axis view, focused on the aortic valve and the aortic root: Blue arrow: ascending aortic (63mm) aneurysm, with effacement of the sino-tubular junction. Panel B: supraesternal echocardiographyc view: an intimal flap, that started at the ascending aorta (white arrow), and progressed to the aortic arch (yellow arrow) and to the braquicephalic trunk (red arrow) is shown.
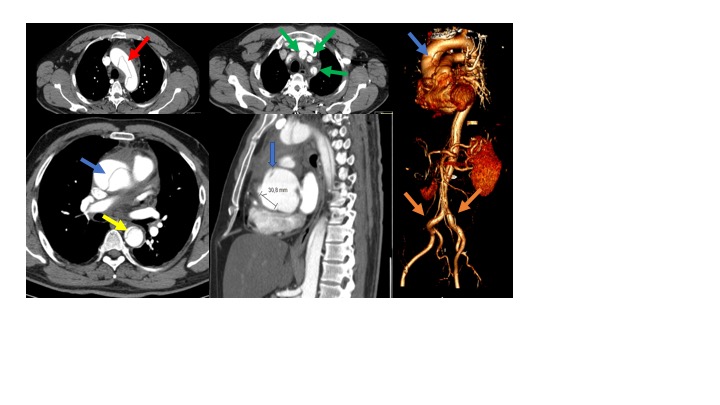
Figura II
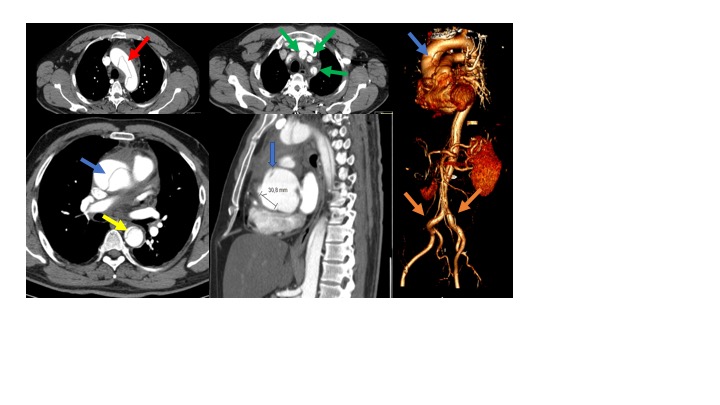
Computed tomographic angiography of the thorax and abdomen revealed an ascending aortic aneurysm (blue arrows) and a type A Stanford aortic dissection. The dissection involved the ascending aorta (blue arrow), aortic arch (red arrow), and descending aorta (yellow arrows), terminating just below the origin of the iliac arteries (orange arrows). Several branch vessels were involved as well, including brachiocephalic artery, left common carotid artery and left subclavian artery (green arrow).
BIBLIOGRAFIA
1-Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ; ESC Committee for Practice Guidelines. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014 Nov 1;35(41):2873-926.
2-Baliga RR, Nienaber CA, Bossone E, OH JK, Isselbacher EM, Sechtem U, Fattori R, Raman SV, Eagle KA: The role of imaging in aortic dissection and related syndromes. JACC Cardiovascular Imaging. 2014 Apr;7(4):406-24
3-Reis L, Almeida I, Teixeira R, Fernandes A, Nascimento J, Gonçalves L: Suprasternal echocardigraphy and aortic dissection. Rev Port Cardiol. 2017 Feb;36(2):151-152
4-Goldstein SA,Evangelista A,Abbara S,Arai A,Asch FM1,Badano LP,Bolen MA,Connolly HM,Cuéllar-Calàbria H2,Czerny M,Devereux RB,Erbel RA,Fattori R, Isselbacher EM, Lindsay JM, McCulloch M, Michelena HI, Nienaber CA, Oh JK, pepi M, Taylor AJ, Weinsalft JW, Zamorano JL, Dietz H, Eagle K, Elefteriades J, Jondeau G, Rousseau H, Schepens M. Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging: endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2015 Feb;28(2):119-82. doi: 10.1016/j.echo.2014.11.015.
5-Arthur J. Labovitz, Vicki E. Noble, Michelle Bierig, Steven A. Goldstein, Robert Jones, Smadar Kort, Thomas R. Porter, Kirk T. Spencer, Vivek S. Tayal, Kevin Wei. Focused Cardiac Ultrasound in the Emergent Setting: A Consensus Statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 2010;23:1225-30.
6-American College of Emergency Physicians. Use of ultrasound imaging by emergency physicians. Policy 400121. Available at: http://www.acep.org. Accessed November 1, 2009.