The majority of peripheral adenopathies are self-limited, the most common cause being infection.1,2 However, their possible etiologies are much wider, including autoimmune disorders and malignancies. 1,2,3 The etiologic approach implies a careful evaluation as the delayed diagnosis of some diseases can have profound and fatal consequences.
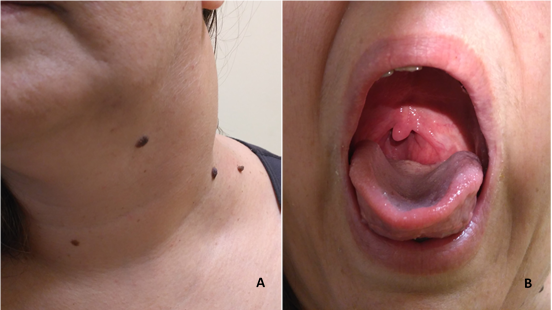
A 45-year-old woman with no relevant medical history, was referred to consultation due to a left cervical tumefaction. The patient referred a sudden appearance of the tumefaction, three weeks previously, no other symptoms, with no evident infectious source. The cervical ultrasound performed at that time revealed a bulky adenopathy, larger than 3cm.She was medicated with amoxicillin/clavulanic acid and a non-steroidal anti-inflammatory, however the tumefaction did not remit. She also complained about the progressive appearance of dysphonia and dysphagia, accompanying the growth of the cervical swelling. The physical examination confirmed the presence of the tumefaction (fig.1A), also revealing an oropharyngeal tumefaction (fig.1B).
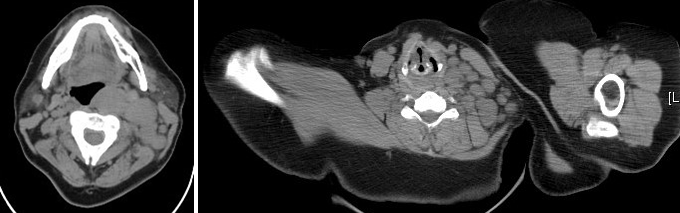
The blood analysis had no alterations, particularly peripheral blood immunophenotyping with no suspicion of lymphoproliferative disease and the negative study of an infectious source. The cervical-thoracic-abdominal-pelvic CT (fig.2) documented left cervical adenopathic formations, the larger with 3cm, molding the floor of the pharynx; as well as the presence of multiple adenopathies in the mediastinum. The lymph node biopsy led to the diagnosis of Classic Hodgkin´s lymphoma, mixed-cellularity subtype. PET revealed lumbar-aortic adenopathies. The patient is currently under chemotherapy, accompanied in Hematology consultation.
The clinical presentation of Hodgkin´s lymphoma is inconstant, but around 70% of patients may present asymptomatic lymphadenopathy.4 Nevertheless, it rarely presents as a bulky adenopathic conglomerate, with no constitutional symptoms. This case demonstrates the importance of biopsy in the study of adenopathies as sometimes it is the only reliable path to the diagnosis. Even when the adenopathy is not easily accessible the biopsy should be performed if possible.
Figura I
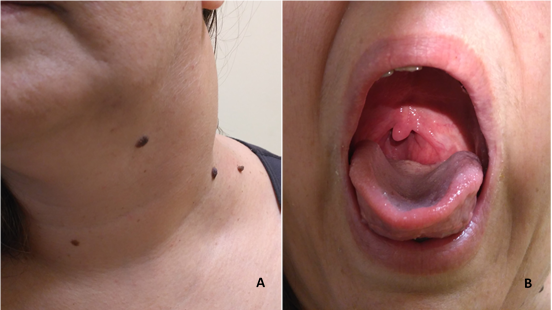
A - Left cervival tumefaction; B - Oropharyngeal examination revealing the pharynx tumefaction
Figura II
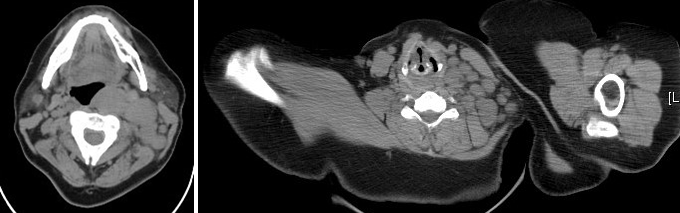
Cervival CT showing a left cervical adenopathic conglomerate, and the adenopathic formations shaping the floor of the pharynx.
BIBLIOGRAFIA
1 Bazemore AW, Smucker DR. Lymphadenopathy and malignancy. Am Fam Physician. 2002; 66(11):2103-10.
2 Ramadas AA, Jose R, Varma B, Chandy ML. Cervical lymphadenopathy: Unwinding the hidden truth. Dent Res J. 2017; 14(1): 73–78.
3 Fletcher RH. Evaluation of peripheral lymphadenopathy in adults. www.uptodate.com. Last update Dec 13, 2016
4 LaCasce AS, Ng AK. Initial evaluation and diagnosis of classical Hodgkin lymphoma in adults. www.uptodate.com. Last update Jul 07, 2017