INTRODUCTION
The posterior reversible encephalopathy syndrome (PRES) is a neurological disorder characterized by varied neurological symptoms, including encephalopathy, seizure, headache, visual disturbances, focal neurological deficits and status epilepticus (1,2). About 40% of all patients require intensive care due to severe complications such as status epilepticus, cerebral ischemia, intracerebral hemorrhage or intracranial hypertension(2).
A leading theory of the pathophysiological changes underlying PRES relates to cerebral blood flow autoregulation response to rapidly developing hypertension and hyperperfusion secondary to failure of those regulatory mechanisms. The posterior brain regions can be particularly susceptible to hyperperfusion because little sympathetic innervation exists in the posterior fossa(2).
Calcineurin inhibitors are reported to be linked with PRES, tacrolimus reaching an average increase of 35% in the mean arterial blood pressure(1). These drugs release vasoconstrictive substances and polymorphisms in the multidrug resistance protein 1 gene may allow its central nervous system dissemination and subsequent neurotoxicity(4).
CASE PRESENTATION
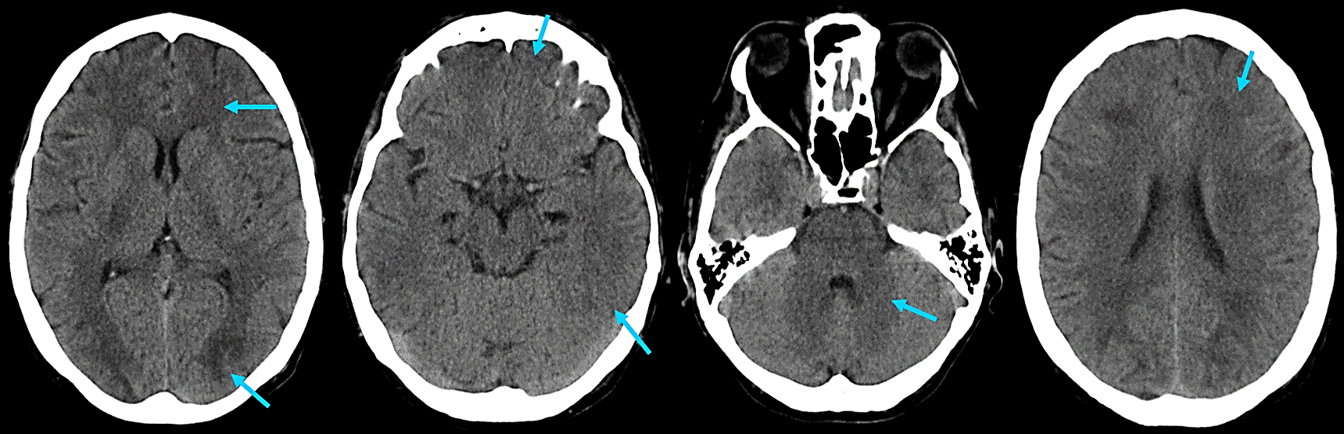
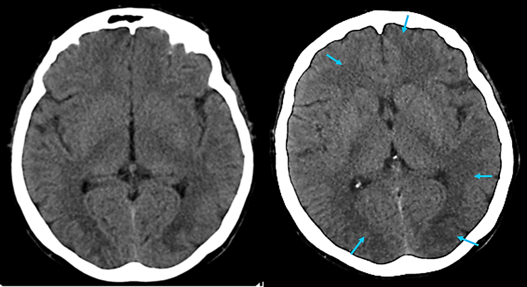
A 40-year-old woman with a background history of Familial Amyloid Polyneuropathy with kidney involvement currently on hemodyalisis, heart involvement carrying a pacemaker and submitted to liver transplantation in 2016, therefore taking tacrolimus 5 mg on a daily basis. Her medications also included ursodeoxycholic acid, pantoprazole, aspirin, sertraline, trazodone and oxazepam. She has history of iodinated contrast allergy. The patient was admitted to the emergency department with headaches and vomiting following hemodialysis session by central venous catheter. On physical examination she was lethargic, dehydrated, afebrile, blood pressure was 160/104mmHg and she had generalized tonic-clonic seizures while waiting for observation, that responded well to endovenous diazepam. No other remarkable points. Head CT scan was performed and showed subcortical bilateral hypodensities in a parieto-occipital dominance but also frontal and corona radiata lesions, without hemorrhage (figure 1). Magnetic resonance imaging (MRI) was not performed because the patient had a pacemaker and serial CT scans (figure 2) showed more defined lesions supporting the diagnosis.
During hospital stay symptoms were successfully controlled with labetalol and tacrolimus was replaced for mycophenolate mofetil resulting in a progressive full clinical recovery with no recurrence of PRES in the follow-up period.
DISCUSSION
PRES is a syndrome that can be found transversally in a variety of medical specialties. The increasing use of neuroimaging led to a higher recognition of this disorder. Neuroimaging, in particular MRI that is superior to CT at diagnosing PRES, frequently shows a distinctive parieto-occipital pattern with a symmetric distribution of changes reflecting vasogenic edema, although it can be normal (2). If MRI is unavailable or contraindicated serial CT brain scanning may be helpful in supporting the diagnosis,(5) such as in this case.
The prognosis is usually favorable(1ľ3) if physicians are aware of this syndrome yielding early recognition and providing apropriate management since delay can result in permanent brain damage and unnecessary interventions.
Ideally, non-invasive continuous monitoring of the cerebrovascular autoregulation may help obtaining the optimal hemodynamic status of these patients during hospital stay but further management of immunosuppressants remains a challenging issue for recurring PRES.
Figura I
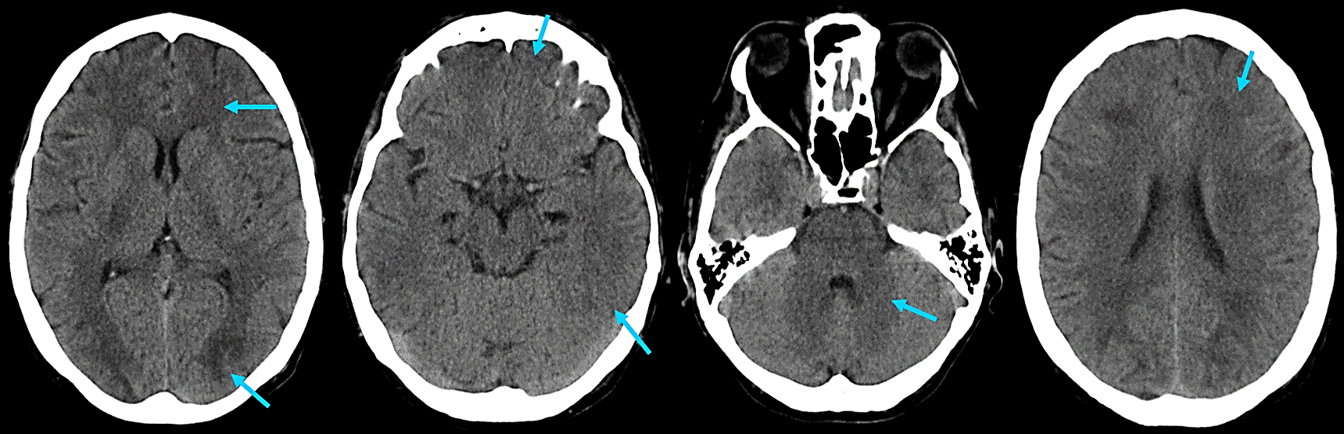
Brain CT scan on day 2: Slightly sharper hypodensities, with a subcortical predominance, visible in the parieto-occipital regions (more expressive to the left) and bilateral frontal regions (blue arrow).
Figura II
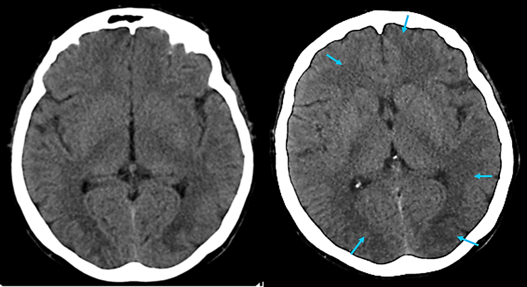
Serial CT scans on day 1 and day 7, respectively, showing more defined lesions (blue arrow).
BIBLIOGRAFIA
1. Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. J Neurol. 2017;264(8):1608ľ16.
2. Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: Clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol [Internet]. 2015;14(9):914ľ25. Available from: http://dx.doi.org/10.1016/S1474-4422(15)00111-8
3. Hinchey J., Chaves C., Appignani B., et al. A Reversible Posterior Leukoencephalopathy Syndrome. NEJM. 1996;494ľ500.
4. Yamauchi A, Ieiri I, Kataoka Y, Tanabe M, Nishizaki T, Oishi R, et al. Neurotoxicity induced by tacrolimus after liver transplantation: relation to genetic polymorphisms of the ABCB1 (MDR1) gene. Transplantation. 2002;74(4):571ľ2.
5. Bartynski WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. Am J Neuroradiol. 2007;28(7):1320ľ7.