INTRODUCTION
Fahr’s syndrome (FS), Fahr’s disease, Idiopathic Basal Ganglia Calcification Syndrome or Bilateral Striatopallidodentate Calcinosis, is a rare neurological disorder that was first described in 1930 by Karl Theodor Fahr. It has a prevalence of less than 1/1000000, and typically presents between the 4th and 6th decades of life 1 . Although it can occur sporadically, FS is most commonly transmitted as an autosomal dominant trait and there are several known causative mutations: SLC20A2 gene on chromosome 8p11.2 2 ; PDGFRB gene on chromosome 5q32 3 ; PDGFB gene on chromosome 22q13.1 4,5 ; XPR1 gene on chromosome 1q25.3 6 . The variability of clinical phenotype underlying this condition makes it a diagnostic challenge.
CASE REPORT
Male, 63 years old, was admitted after a suicidal attempt by hanging. According to his family, a year prior to admission, the patient started with a depressive mood, crying spells, anhedonia, increased sleep and anorexia. After a quarrel with his 90-year-old mother, he decided to commit suicide. He had no history of neurologic deficits, convulsions, syncope or trauma. Except for signs of malnourishment (Body Mass Index of 15.6 kg/m2), his physical examination was normal, and he showed no evidence of movement disorders (tremor, dystonia, ataxia, chorea, athetosis) or memory loss.
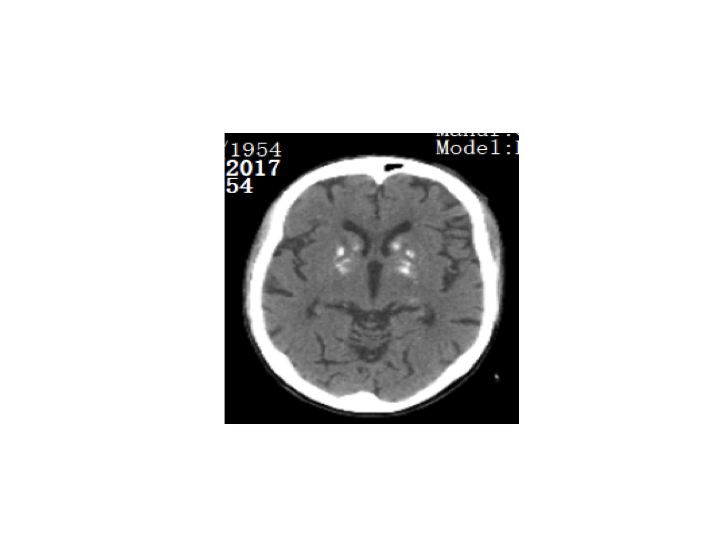
A cerebralcomputed tomography (CT) scan showed profound bilateral calcifications of thebasal ganglia (Figure 1).Complete blood count,C-reactiveprotein, lactic acid,renal and hepatic functions, total plasma parathyroid hormone, calcium, phosphorusand immunological panel(antinuclear antibodies; anti-DNA; anti-SM; antiphospholipid antibody) werenormal. Humanimmunodeficiency virus, Epstein-Barr virus and VDRL tests were negative.Urinary heavy metals dosages were within reference levels.Cerebral spinal fluid cellcount, glucose and proteins were normal and cultures were sterile. A moleculargenetic testing wasn’t performed due to financial constraints. His familyhistory couldn’t, also, be fully accessed for any pattern of inheritance: hisfather had died of “cardiac arrest” when the patient was 12 years old and thereweren’t any paternal relatives. His mother, two maternal uncles and threecousins had a normal clinical examination and cerebral CT scan. The patient hadno offspring.
He was treated with sertraline 100mg/day. There was a progressive improvement in his depressive complaints and no signs of suicidal ideology. He was discharged home, after 2 months-admission, with follow-up appointments scheduled with his psychiatrist.
DISCUSSION
The typical presentation of FS is a parkinsonian or choreoathetotic type movement disturbance but it can also be associated with seizures, epilepsy, headache, dysarthria and spasticity. Neuropsychiatric manifestations are also common presenting symptoms and can range from mild cognitive impairment to dementia, psychosis, personality or behaviour changes7.
Symmetric calcifications result from abnormal deposition of calcium and can be seen in the basal ganglia, more specifically in the internal globus pallidus, caudate, putamen, dentate nuclei, and thalamus1. Recent studies suggest that the extent of calcification predicts neuropsychiatric disorders but not neurological deterioration8.
Diagnostic criteria of Fahr’s syndrome has been modified and derived from Manyam et al.9(2005) and it can be stated as follows: bilateral basal ganglia calcifications; progressive neurologic dysfunction; family history of basal ganglia calcifications with an autosomal dominant pattern of inheritance; absence of another condition that could explain the calcifications such as metabolic (in particular parathyroid disturbances), mitochondrial, infectious, toxic or traumatic causes.
To date, no curative treatment exists for Fahr´s syndrome because there isn’t any method to selectively remove the deposited calcium from the brain without affecting the calcium from bones and other tissues1. Management strategies focus on symptomatic relief. In this case, the patient started with an antidepressant. Considering the rarity of the condition and the limited cases available in the Literature for therapeutic guidance, it is not possible to recommend one drug over another and more studies need to be conducted.
Prognosis is variable, cannot be predicted and is unrelated to the extent of calcification. Death usually occurs secondary to neurological deterioration10.
In conclusion, this report shows a case of sporadic Fahr’s syndrome that presented with depression and no neurological deficits. Since other etiologies were ruled out and the typical calcifications were present, it also illustrates the necessity for a heightened awareness of this uncommon disease and the importance of brain imaging in psychiatric patients.
Figura I
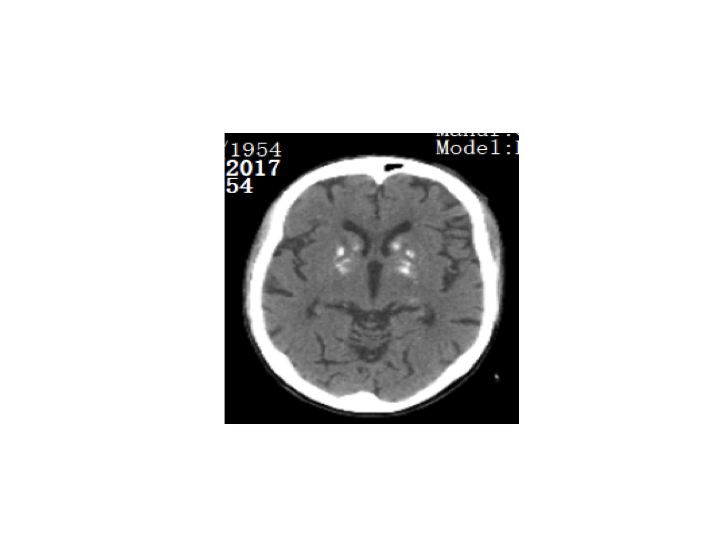
Profound Bilateral Calcifications of the Basal Ganglia
BIBLIOGRAFIA
REFERENCES
1. Manyam BV, Walters AS, Narla KR. Bilateral Striatopallidodentate calcinosis: clinical characteristics of patients seen in registry. Movement Disorders: official journal of Movement Disorder Society 2001, 16(2): 258- 264
2. Wang C, Li Y, Shi L, Ren J, Patti M, Wang T et al. Mutations in SCLC20A2 link familial idiopathic basal ganglia calcification with phosphate homeostasis. Nat Genet 2012; 44:254
3. Nicolas G, Pottier C, Maltête D, Coutant S, Rovelet-Lecrux A, Legallic S et al. Mutation of the PDGFRB gene as a cause of idiopathic basal ganglia calcification. Neurology 2013; 80:181
4. Keller A, Westenberger A, Sobrido MJ, Garcia-Murias M, Domingo A, Sears RL et al. Mutations in the gene encoding PDGF-B cause brain calcifications in humans and mice. Nat Genet 2013; 45:1077
5. Keogh MJ, Pyle A, Daud D, Griffin H, Douroudis K, Eglon G et al. Clinical heterogeneity of primary familial brain calcification due to a novel mutation in PDGFB. Neurology 2015; 84:1818
6. Legati A, Giovannini D, Nicolas G, López-Sánchez U, Quintás B, Oliveira JR et al. Mutations in XPR1 cause primary familial brain calcification associated with altered phosphate export. Nat Genet 2015; 47:579
7. Saleem S, Aslam HM, Anwar M, Anwar S, Saleem M, Saleem A et al. Fahr’s syndrome: literature review of current evidence. Orphanet J Rare. 2013, 8:156. 10.1186/1750-1172-8-156
8. Claussen MC, Hassanpour K, Jenewein J, Boettger S. Familial idiopathic basal ganglia calcification (Fahr’s syndrome): initial clinical neuropsychiatric presentation without corresponding neurological deficit. Int Neuropsychiatr Dis J 2017: 9:1-5
9. Manyam BV. What is and what is not ‘Fahr’s disease.’ Parkinsonism. Relat. Disord 11(2), 73-80 (2005)
10. Rastogi R, Singh AK, Rastogi UC, Mohan C, Rastogi V. Fahr’s syndrome: a rare clinic-radiologic entity. Med J Armed Forces India 2011; 67(2): 159-161