Introduction
Lyme borreliosis is a tick-borne infection caused by Borrelia burgdoferi sensu lato complex spirochetes. It is the most common zoonosis in Western Europe with an estimated incidence of 22/100000 person-year1. In Portugal 53 cases have been declared between 2013-2016, though it is believed that there is significant sub-diagnosis2.
It is predicted that around 10-15% of patients will develop neurologic manifestations3. The most common presentations of Lyme neuroborreliosis (LNB) are lymphocytic meningitis, cranial neuritis or radiculoneuritis, isolated or as a group4.
Spinal cord involvement is extremely rare but when it occurs it commonly presents as diffuse or multifocal T2-weighted cord lesions on Magnetic Resonance Imaging (MRI) 3.
We report one patient with sensory ataxia as the main manifestation of LNB.
Case presentation
A 54-year-old woman with background of depression and arterial hypertension was admitted to the Emergency Department (ED) for progressive gait and sensitivity disturbances developing throughout almost a year.
In the Emergency Department, the neurological exam shown peripheral paraesthesia, abolishment of profound sensitivity in the upper and lower limbs, ataxic gait with need for bilateral support, dysmetria in the finger-to-nose test and positive Romberg test. It was decided to admit the patient on the Medical Ward for aetiological investigation.
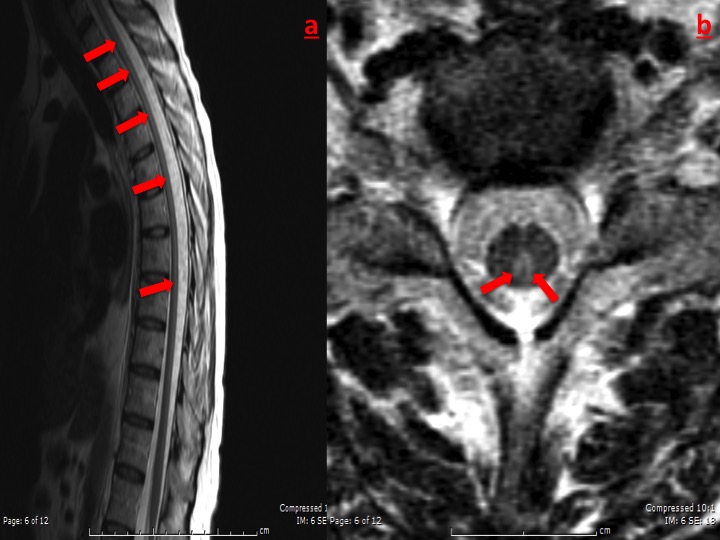
Spinal MRI showed linear hyperintense T2 signal centromedular along the dorsal segment, with cervical extension, predominantly in the posterior cord with no apparent enhancement after contrast.(Fig.1)
Lumbar puncture revealed acellular liquor without significant glucose consumption (40%) and mildly elevated proteins (58mg/dL). No oligoclonal bands were detected.
An exhaustive screening for infectious (human immunodeficiency virus [HIV], hepatitis C viruses [HCV], syphilis and Borrelia serology), autoimmune (antinuclear, extractable nuclear antigen and double stranded desoxyribonucleic acid antibodies), metabolic (seric copper, ceruloplasmin, folate, vitamin B12, homocysteine, methylmalonic acid and thyroid function) or neoplastic causes (thoracic, abdominal and pelvic Computed Tomography scan) was done, and the only relevant results were a low folate level (1,1 ng/mL), an equivocal B.burgdoferi IgG with positive IgM serology by ELISA (Enzyme-linked immunosorbent assay) and abnormal evoked potentials.
It was assumed a combination between folate deficiency and a demyelinating disease (mildly elevated liquor proteins, sensory ataxia, MRI pattern and abnormal evoked potentials, suggested multiple sclerosis). A 5-day cycle of pulsed corticotherapy and folate supplementation was tried with no symptomatic improvement.
Given the unsuccessful treatment it was decided to restart the investigation searching for other aetiology. Reviewing the background story, even though the patient never detected any tick-bite stigma, she worked in a school surrounded by tall grass and was her habit to cross it when exiting her workplace. So, it was decided to repeat the serology, this time by the Western Blotting test, which was positive for B.burgdoferi IgG.
Lumbar puncture was repeated and positive IgG B.burgdoferi was detected, with the same method, supporting the diagnosis of LNB.
A regimen of 30 days of ceftriaxone was done with minor improvement and patient was discharged for outpatient follow-up with regular physical rehabilitation (at discharge patient had total incapacity to walk).
During the first six month follow-up there was a frank amelioration in the gait and paresthesia. After one-year all the spinal MRI abnormalities had disappeared and now, almost three years after hospital admission the patient is able to walk autonomously with the help of a single crutch.
Discussion
Myelitis is a very rare manifestation of Borrelia infections. This diagnosis is based on clinical and imagiological evidence of myelitis, evidence of Borrelia presence in the cerebrospinal fluid (CSF) and active exclusion of other causes.5
The diagnosis of sensory ataxia (SA) is very challenging and one that often elicits confusion with cerebellar ataxia (CA). Nystagmus and dysarthria, for instance, are very common in CA and extremely rare in SA. Contrarily finger-nose and heel-shin ataxia, joint position sense impairment, exteroceptive sensation reduction and positive Romberg sign are characteristics of SA and not CA. The gait is also diverse, with a high stepping, unstable gait in SA and broad-based staggering gait in CA.
This patient presented limb paraesthesia, gait disorders with sensory ataxia, loss of proprioception and spastic paraparesis which were very suggestive of lesion on dorsal columns.6Other aetiologies that seldom relate to SA in this anatomical region are vitamin B12 or copper deficiency, tabes dorsalis, cervical myelopathy and myelitis related to HIV or HCV.6
To assume the diagnosis of LNB there has to be: a) probability of exposure; b) clinical evidence of neurologic disease; c) laboratory tests that support the diagnosis 4. This patient had risk for exposure, presented neurologic clinical features and CSF compatible with LNB. It is essential to have an abnormal CSF, preferably with pleocytosis and some direct or indirect evidence of Borrelia presence. Frequently the bacterial load is very low in accessible fluid and so, the Polymerase Chain Reaction methods have very low sensitivity. So, the investigation must be focused in antibody detection. Unfortunately those tests also have some limitations 4 namely: a) it takes around 2-4 weeks to have a significative antibody response; b) test may remain positive indefinitely after successful treatment; c) antigenic similarities with other organisms, like Treponema.
So, a two-tier method should be used to increase diagnostic accuracy 4. The first should be an ELISA test and, if borderline or positive, a secondary test with Western Blotting should be done. A double positive test is highly suggestive of present or past contact with Borrelia. The method should be the same for serum or CSF investigation.
LNB is very antibiotic responsive and most of the nervous system inflammation can be solved with timely antibiotherapy. The suggested treatment7is doxycicline 100-200mg, oral, twice a day or ceftriaxone 2g, endovenous, once a day. If the disease is limited to peripheral nerves or meninges, both options are equally effective, if there is parenchymal disease parenteral antibiotics should be preferred.
With this case the authors intended to present the diagnostic challenge of this rare aetiology for sensitive ataxia and present a small review of this disease. It was shown not only a rare and debilitating disease but also one that, if correctly and readily diagnosed, could dramatically change the patientĺs quality of life.
Figura I
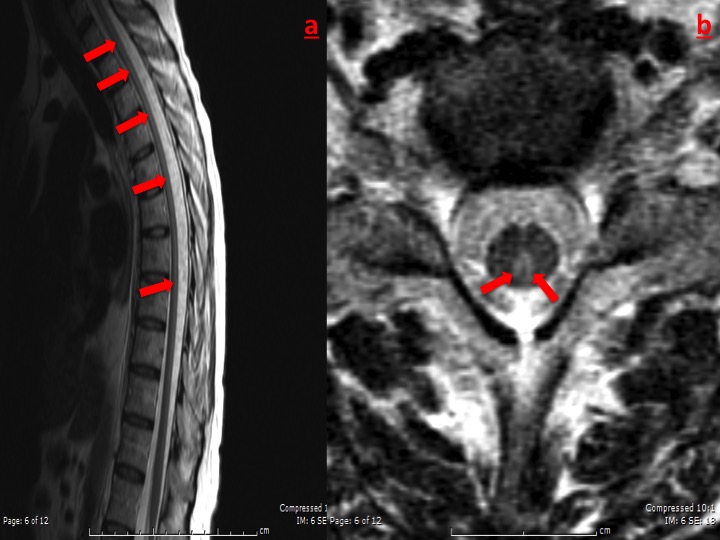
Spinal Cord MRi, sagittal (a) and axial (b) view, showing linear hyperintense T2 signal along the dorsal segment, with cervical extension, predominantly in the posterior cord.
BIBLIOGRAFIA
1- Skyes RA. An estimate of Lyme borreliosis incidence in Western Europe. J Public Health. Volume 39, Issue 1, 1 March 2017, Pages 74ľ81,
2- Direcção-Geral da Saúde (DGS), DirešŃo de Servišos de InformašŃo e Anßlise DivisŃo de Epidemiologia e VigilÔncia. Doenšas de DeclarašŃo Obrigatˇria, 2013-2016 - Volume II, 2017 (http://www.dgs.pt/).
3- Hildenbrand P ,Craven DE, Jones R, Nemeskal P. Lyme Neuroborreliosis: Manifestations of a Rapidly Emerging Zoonosis. Am J Neuroradiol. 2009; 30:1079ľ87
4- Halperin JJ. Diagnosis and management of Lyme neuroborreliosis. Expert Rev Anti Infect Ther.2018;16(1):5-11.
5- Brßs A,Marques N,Santiago B,Matos A,Moreira F. Extensive Myelitis as a Manifestation of Neuroborreliosis. Acta Med Port.2016;29(9):564-566
6- Chhetri SK, Gow D, Shaunak S, Varma A. Clinical assessment of the sensory ataxias; diagnostic algorithm with illustrative cases. Pract Neurol.2014; 14(4):242-51.
7- Mygland A, Ljostad U, Fingerle V, et al. EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis. Eur J Neurol. 2010;17(1):8ľ16, e1ľ4.