A 28-year-old girl presented to our emergency department with a 24-hour history of nausea, post-prandial emesis and abdominal pain. The patient recalled a history of similar episodes in the last 5 years. These episodes usually lasted 2-3 days, spontaneously remitted and became more frequent in last year, which led to a 3Kg weight lost. There was no hematuria or flank pain. At admission she was afebrile and hemodynamically stable; physical examination revealed a distended abdomen with generalized tympanism and epigastric pain but with no guarding or rebound tenderness. Laboratory findings were remarkable for a neutrophilic leukocytosis and mild hypokalemia. There was no proteinuria. An abdominal and pelvic CT scan revealed gastric and duodenal dilation with the third duodenal portion being compressed by the superior mesenteric artery, suggesting Wilkie’s syndrome (Fig. 1). In addition, the left renal vein was compressed by the superior mesenteric artery in its ending (Fig. 2) - nutcracker phenomenon. A nasogastric tube was placed for gastric decompression and fluid and electrolyte replacement was initiated. The patient was discharged home the next day and was advised to eat a fractionated diet and assume a slightly prone position while eating. After surgical consultation, conservative management was maintained, and the patient remains asymptomatic at 2 years’ follow-up. Superior mesenteric artery syndrome, also called Wilkie’s syndrome, is a rare cause of duodenal obstruction. It results from exterior compression of the third duodenal portion by the overlying superior mesenteric artery, which in these cases originates from the abdominal aorta in an unusually narrow angle.
1 Nutckracker phenomenom or syndrome (when signs or symptoms are present) consists of renal vein compression between the aorta and the superior mesenteric artery.
2 Hematuria, flank pain and proteinuria can ensue. We report a patient with the simultaneous occurrence of Wilkie’s syndrome and nutcracker phenomenon, an event quite rare with only a few case reports in the literature.
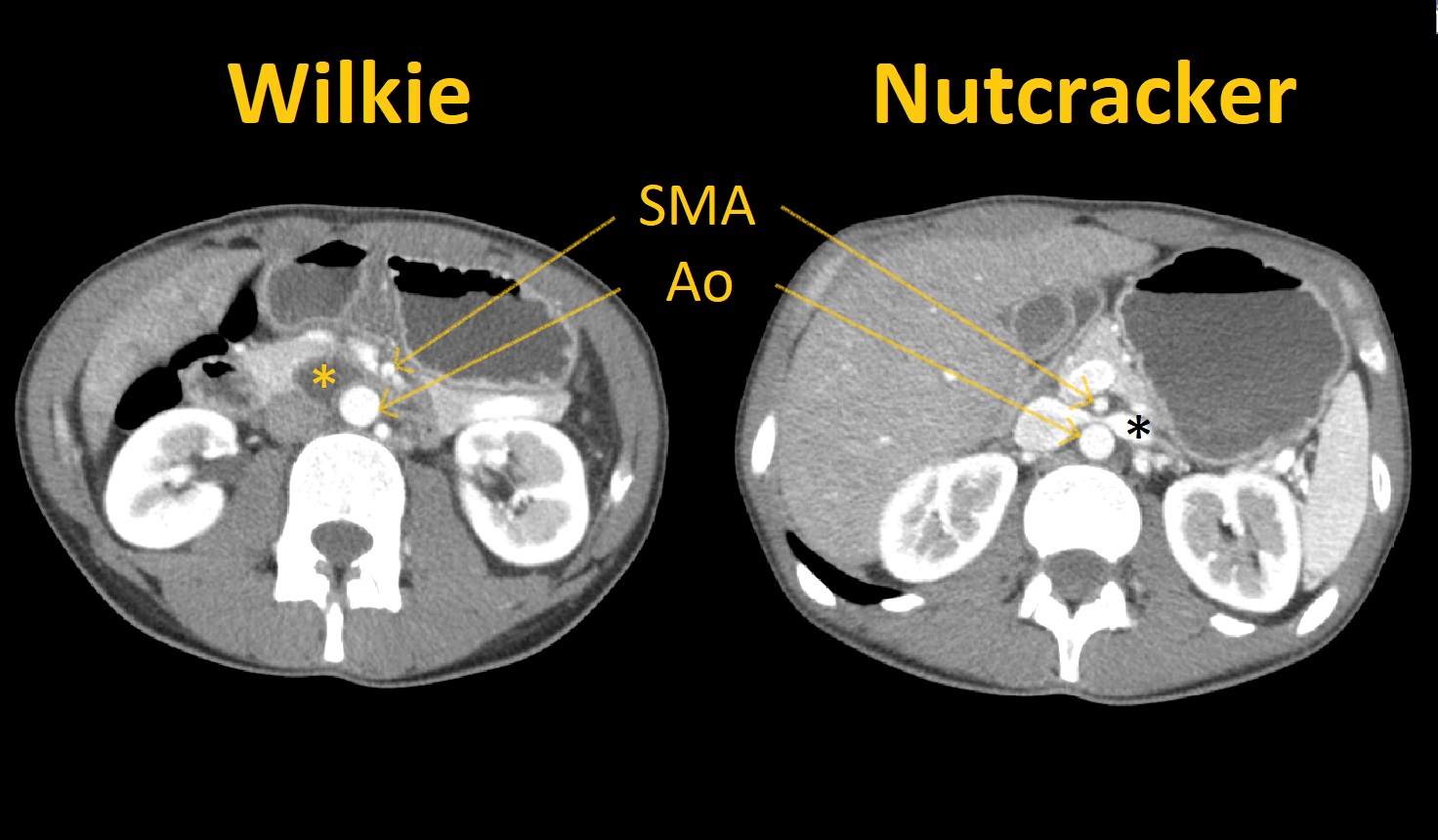
3-6Figura I
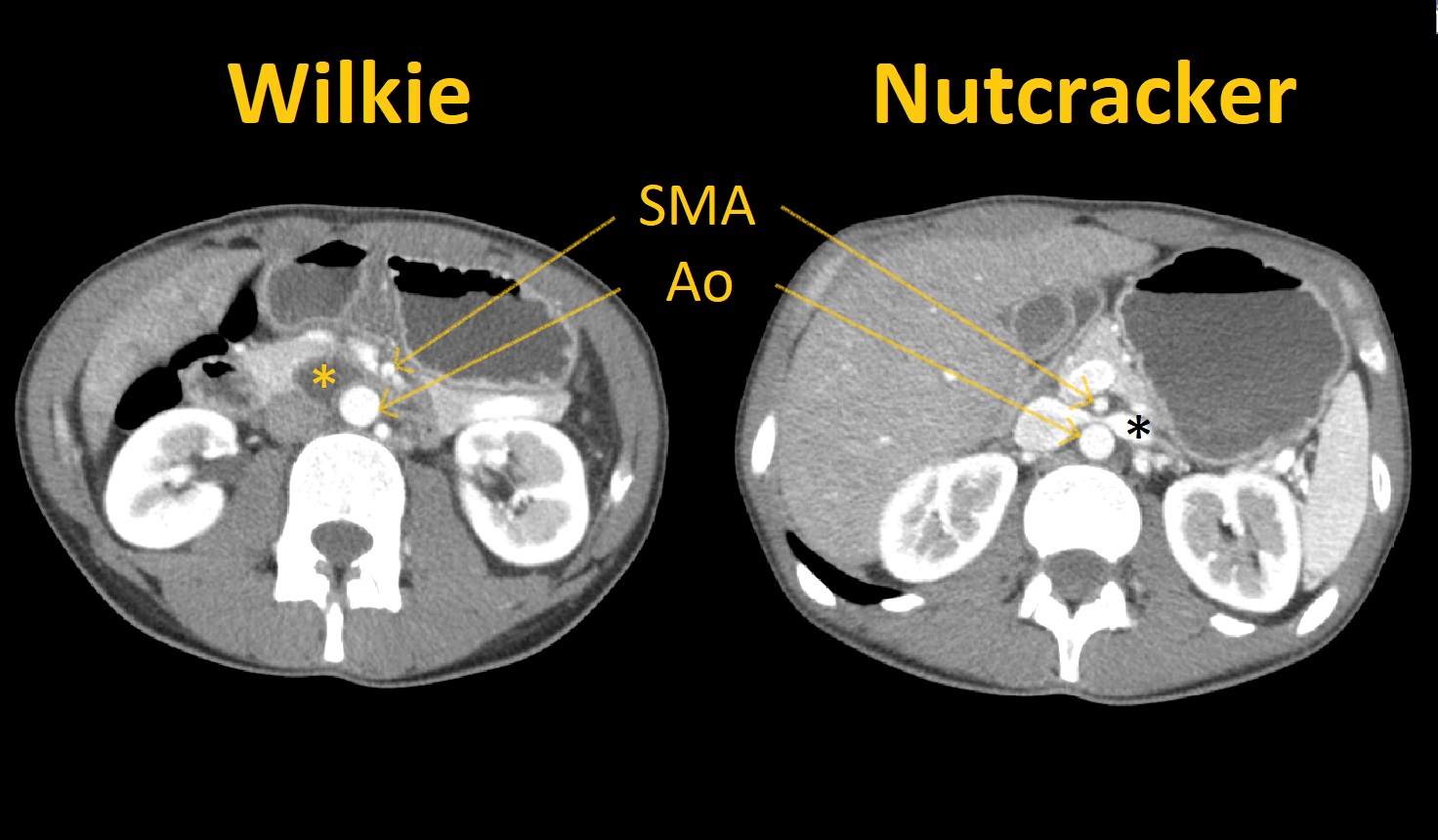
Figure 1. Patient abdominal and pelvic computed tomography with coincident Willkie syndrome and Nutcracker phenomenon. Left image –showing superior mesenteric artery (SMA) compressing duodenum (yellow asterisks) against abdominal aorta artery (Ao) with duodenal and gastric dilatation. Right image –left renal vein (black arrow) compression by SMA.
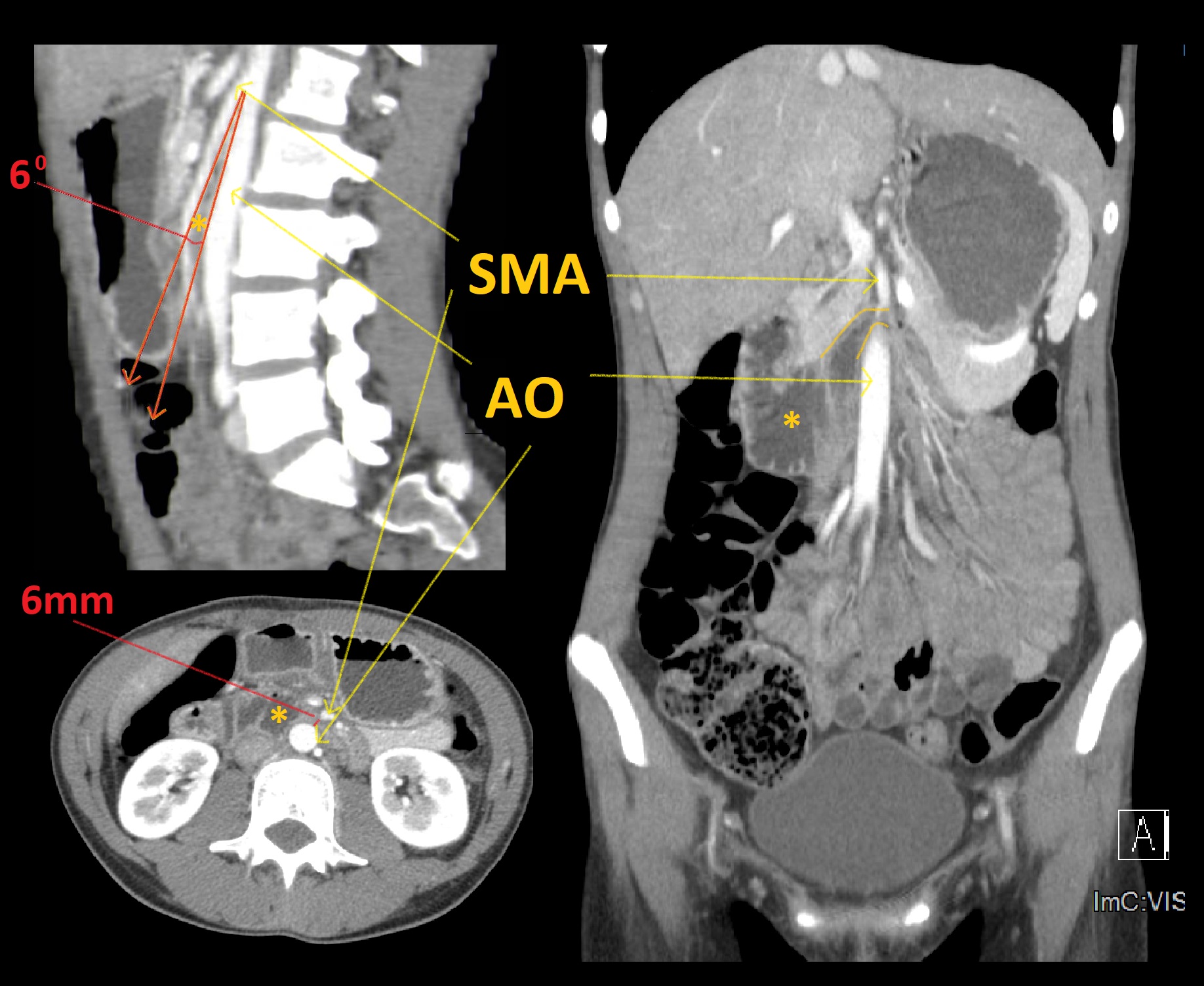
Figura II
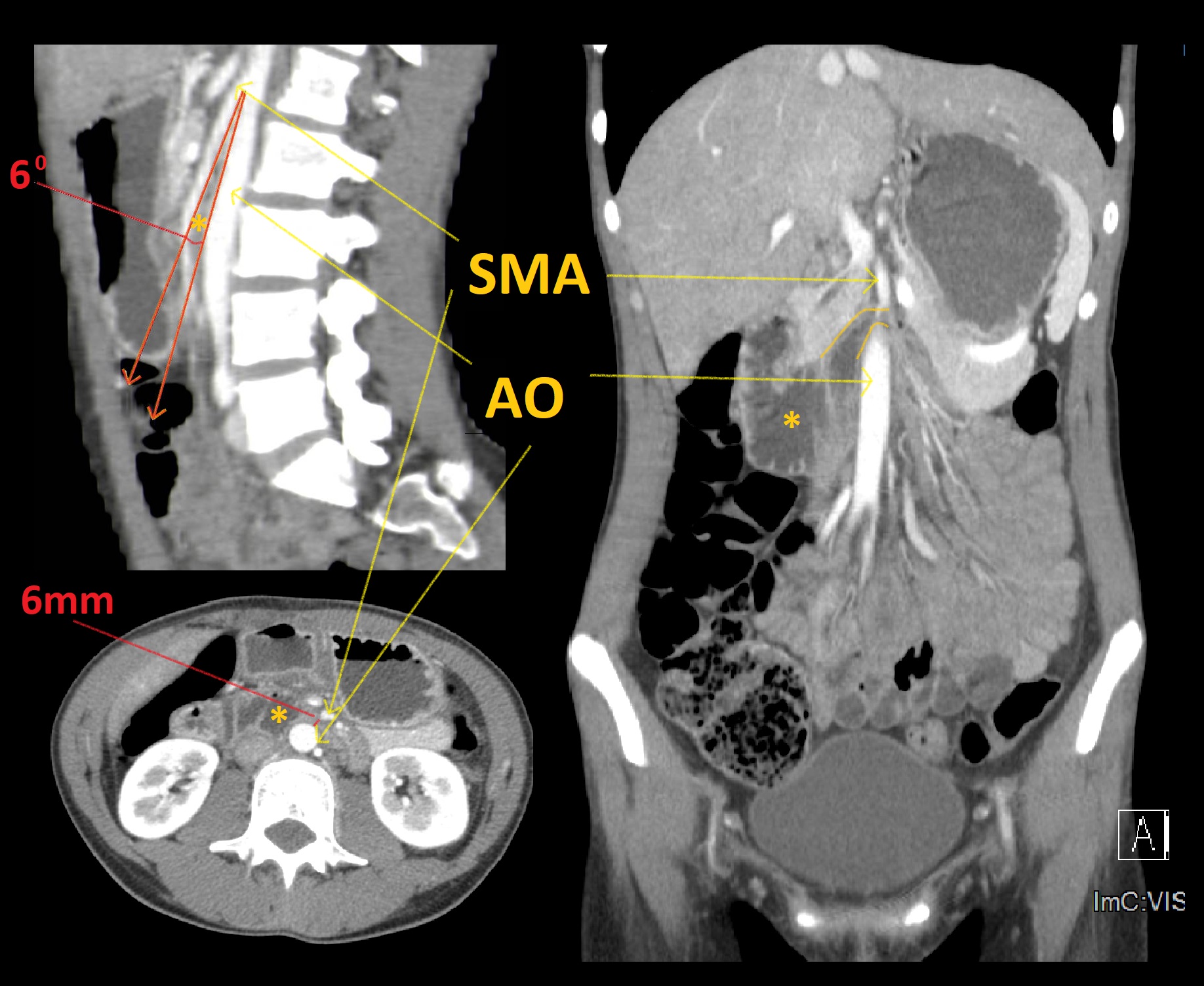
Figure 2. Patient abdominal and pelvic computed tomography. Upper left – sagittal plane showing a 6° angle (normal 25-60°) between superior mesenteric artery (SMA) and abdominal aorta (Ao) compressing duodenum (yellow asterisk). Bottom left - axial plane showing a 6mm distance between SMA and Ao (normal 10-28 mm). Right – coronal plane showing duodenal compression between Ao and SMA. There is proximal duodenal dilatation.
BIBLIOGRAFIA
1. Mandarry MT, Zhao L, Zhang C, Wei ZQ. A comprehensive review of superior mesenteric artery syndrome. Eur Surg. 2010;229–36.
2. Gulleroglu K, Gulleroglu B, Baskin E. Nutcracker syndrome. World J Nephrol. 2014 3(4):277–81.
3. Heidbreder R. Co-occurring superior mesenteric artery syndrome and nutcracker syndrome requiring Roux-en-Y duodenojejunostomy and left renal vein transposition: a case report and review of the literature. J Med Case Rep. 2018 12(1):214.
4. Michael PG, Al-Saadi T, Jamkhandikar R. A Rare Case of Coexisting Superior Mesenteric Artery Syndrome and Nutcracker Phenomenon. Sultan Qaboos Univ Med J. 2017 17(3):e368–70.
5. Nunn R, Henry J, Slesser AAP, Fernando R, Behar N. A Model Example: Coexisting Superior Mesenteric Artery Syndrome and the Nutcracker Phenomenon. Case Rep Surg. 2015;649469.
6. Vulliamy P, Hariharan V, Gutmann J, Mukherjee D. Superior mesenteric artery syndrome and the “nutcracker phenomenon”. BMJ Case Rep. 2013