A 61 years-old male presented to the emergency department with new-onset generalized tonic-clonic seizures. His previous medical history included acral vitiligo and cataract surgery. He had no history of alcohol or drug abuse, fever, headache or head trauma. His family history was irrelevant.
The physical exam revealed depigmented macules confined to the distal extremities. There were no neurologic deficits nor additional pathological findings.
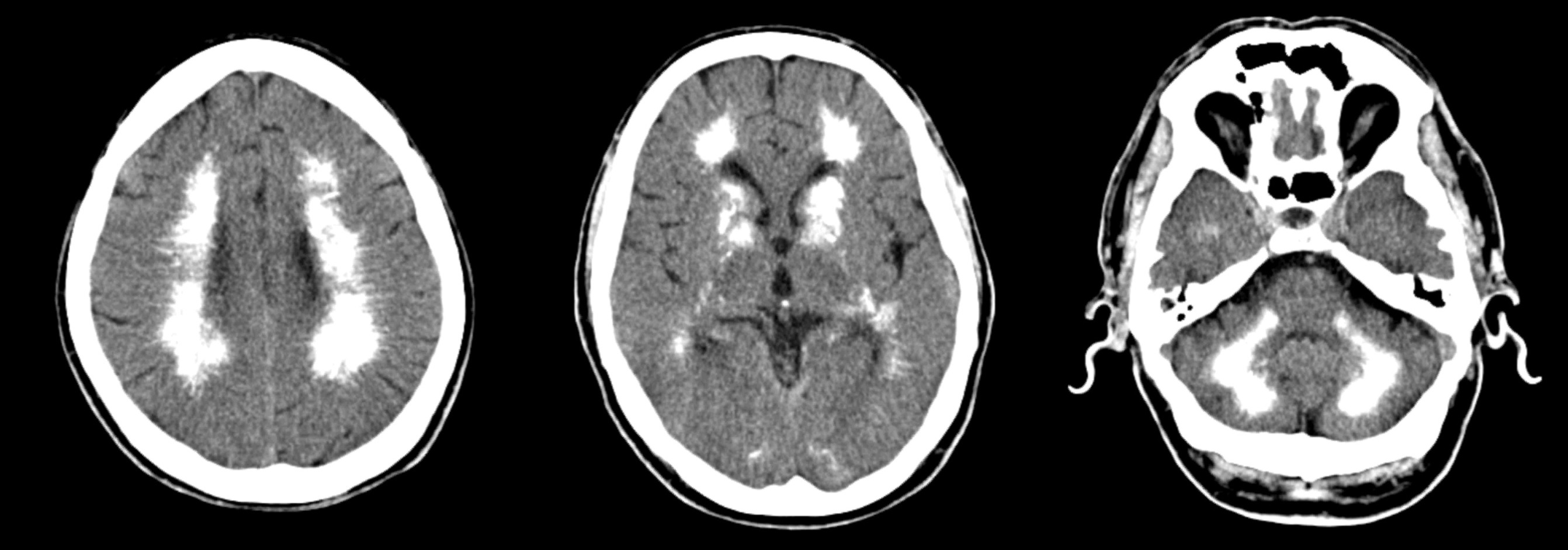
Head CT showed extensive symmetrical cerebral calcification affecting subcortical white matter, thalami and basal ganglia (Figure 1).
The workup uncovered low total and ionized serum calcium, elevated phosphorus and normal serum PTH, 24-hour calcium excretion, alkaline phosphatase, magnesium, creatinine, albumin, 25-hydroxyvitamin D, cortisol and ACTH levels. Thyroid function was normal. Thyroid, ANA and ANCA antibodies and HIV were negative. We have found no evidence of diabetes or parathyroid glands’ infiltrative diseases.
A diagnosis of idiopathic primary hypoparathyroidism was considered. However, the normal range (albeit inappropriately low) PTH levels, the high normal urinary calcium excretion rather than the expected low excretion in the presence of hypocalcemia, the non-syndromic presentation in late adulthood led us to question this hypothesis and to consider a possible calcium-sensing receptor (CaSR) disorder1. Although we favor the possibility of a CaSR disorder it’s rather difficult, based on the measurements of serum PTH and urinary calcium, to distinguish this entity from hypoparathyroidism.
As this was a sporadic case, the patient has no descendants and the diagnostic confirmation will not change our therapeutic strategy or the patient prognosis, we have decided to dispense the genetic testing.
The patient received calcium and vitamin D supplementation to maintain serum calcium level (albumin adjusted total calcium or ionized calcium) in the lower part or slightly below the lower limit of the reference range.2 So far, the patient remains stable without treatment complications namely renal stones, nephrocalcinosis, and renal insufficiency.
Figura I
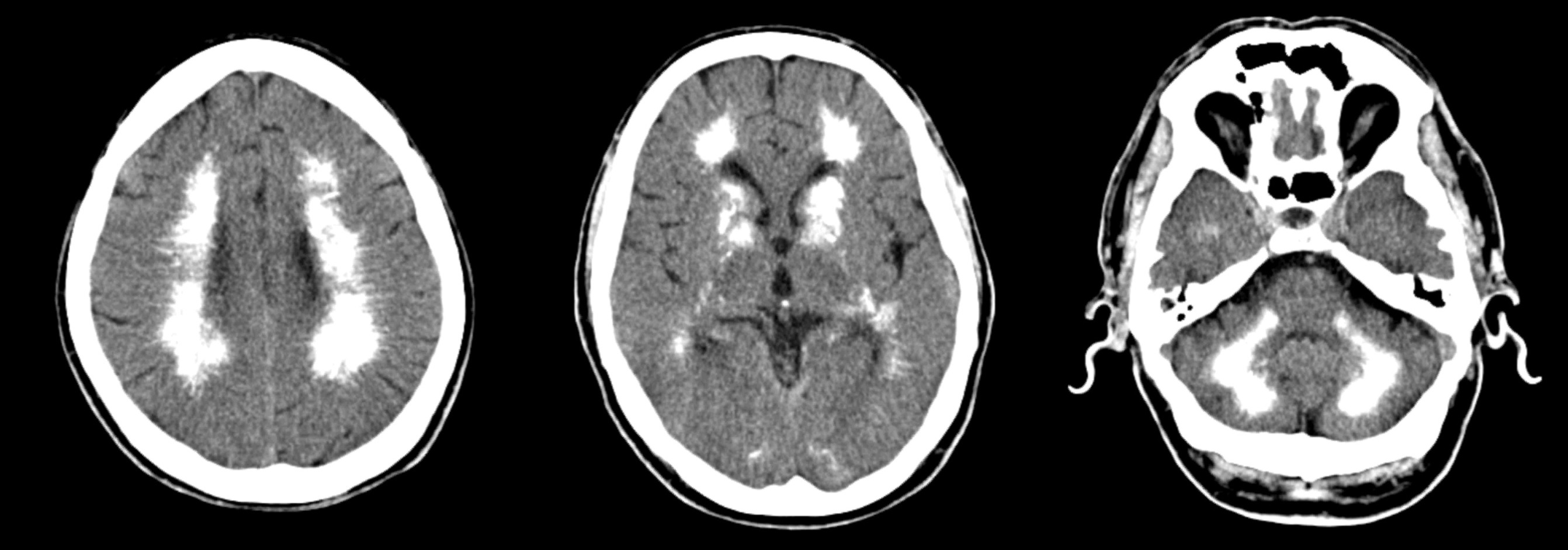
Head CT images showing centrum semiovale, basal ganglia and dentate nucleus calcification.
BIBLIOGRAFIA
1- Pearce SH, Williamson C, Kifor O, Bai M, Coulthard MG, Davies M, Lewis-Barned N, McCredie D, Powell H, Kendall-Taylor P, Brown EM, Thakker RV. A Familial A familial syndrome of hypocalcemia with hypercalciuria due to mutations in the calcium-sensing receptor. N Engl J Med. 1996 Oct 10;335(15):1115-22
2-Bollerslev J, Rejnmark L, Marcocci C, Shoback D, Sitges-Serra A et al. European Society of Endocrinology Clinical Guideline: Treatment of chronic hypoparathyroidism in adults. European Journal of Endocrinology (2015) 173, G1–G20.