Introduction
De Quervain’s thyroiditis is an uncommon cause of thyrotoxicosis but the most common cause of a painful thyroid gland. It affects women more likely than men and the average age of onset is 30 to 50 years1. Pain is the most common presenting and dominating symptom2, usually accompanied by other symptoms as fever, fatigue, anorexia and myalgia. The diagnosis is essentially clinical, but when the clinical manifestations are less obvious, laboratorial and imaging studies are needed for differential diagnosis. During the early stage, thyroid hormones and erythrocyte sedimentation rate (ESR) are elevated and less frequently mild anaemia and abnormal liver function tests may be present3. The ultrasonography shows a diffusely or focally hypoechogenic gland and is useful in excluding other diagnosis as abscesses, haemorrhage or nodules. In addition, if necessary, a radioiodine or technetium imaging study showing low uptake of radionuclide confirms the diagnosis. Regarding treatment, therapy with antithyroid drugs is not indicated, beta blockers may be indicated for the symptomatic treatment of hyperthyroidism symptoms and anti-inflammatory drugs are effective in analgesia.
Case report
We describe the case of a 54-year old woman with history of pulmonary tuberculosis (PT) in childhood and acute herpes zoster of the left cervical region with postherpetic neuralgia two years prior to the admission in our hospital. There was a recent contact with a relative with PT, four months prior to our observation. She presented with left anterior cervical discomfort and tumefaction over the past eight weeks, associated in the last three weeks with left frontotemporal headache, vespertine fever, night sweats, malaise, myalgia, anorexia and significant weight loss (9% of total body weight). She denied palpitations, insomnia, tremors, or the appearance of any rash, jaw claudication, visual disturbances, as well as urinary, respiratory or abdominal symptoms.
On observation, the patient was pale, apyretic, eupnoeic, with normal arterial blood pressure 111/62mmHg but steadily tachycardic with 110 beats per minute. Cervical palpation revealed an enlarged and tender thyroid gland without other local inflammatory signs, no palpable nodules, temporal artery was not palpable and cardiopulmonary auscultation was normal.
Laboratory results revealed an inflammatory normocytic normochromic anaemia with haemoglobin 10.6g/dL, ferritin was elevated 312.4μg/L (normal range 10.0 to 120.0μg/L), sideraemia, transferrin saturation, vitamin B12 and folic acid were normal. ERS and C-reactive protein (CRP) were elevated: VS 124mm/h (normal <30mm/h) and CRP 3.45mg/dL (normal <0.5mg/dL). Plasmatic protein electrophoresis was normal. Mild elevation of liver biochemical tests less than two times the upper limit of normal (aspartate aminotransferase 25UI/L, alanine aminotransferase 67UI/L, gamma-glutamyl transferase 118UI/L, alkaline phosphatase 151UI/L). A viral, bacterial and protozoal serologies panel was performed (including HIV, hepatitis B and C, Herpes simplex 1 and 2, Cytomegalovirus, Toxoplasma gondii, Brucella spp, Rickettsia conorii, Rickettsia rickettsia, Rickettsia typhi, Coxiella burnetti and Leishmania donovani), all negative except evidence of past Herpes simplex 1 and Cytomegalovirus contact (IgG+/IgM-). Blood cultures were negative. Thyroid function tests showed a suppressed thyroid stimulating hormone (TSH) level of <0.01mUI/L (normal range 0.27 to 4.2mUI/L) and elevated levels of free thyroxine (fT4) 72.1pmol/L (normal range 12.0 to 22.0pmol/L), total triiodothyronine 5.88nmol/L (normal range 0.9 to 2.8nmol/L) and free triiodothyronine 22.9pmol/L (normal range 3.5 to 6.5pmol/L). Anti-thyroglobulin, anti-thyroid peroxidase, and anti-thyrotropin receptor antibodies were negative. Antinuclear antibodies test was negative.
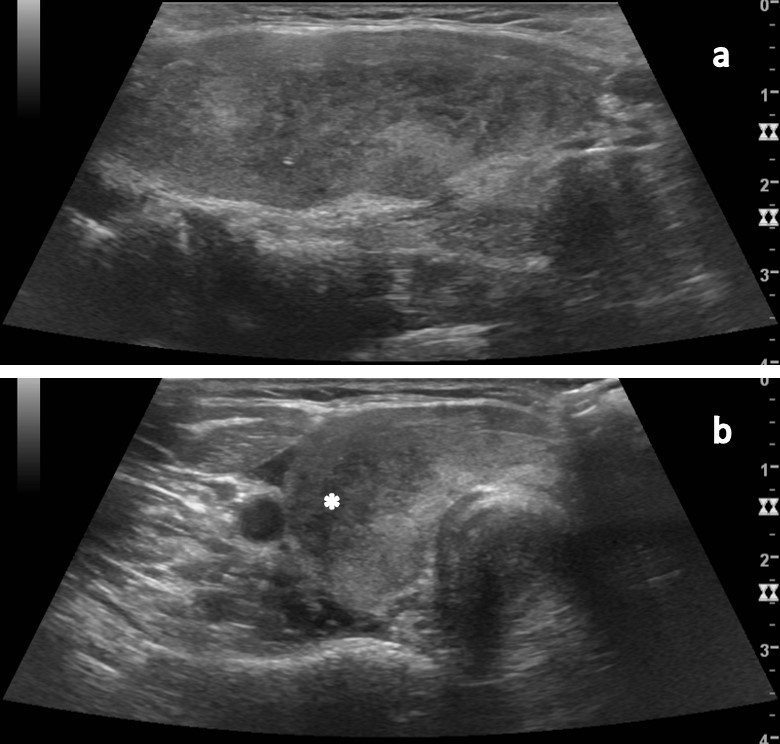
The cervical ultrasonography (US) revealed a globose gland with a diffusely and heterogeneous structure, with bands of hypoechogenicity, suggestive of subacute/chronic thyroiditis (Fig. 1).
An abdominal US and thoracic, abdominal and pelvic computed tomography (CT) scan showed no significant alterations, specifically absence of enlarged lymph nodes or parenchymal nodules of the lung, liver or spleen.
The diagnosis of subacute thyroiditis was made and the patient was started on nonsteroidal anti-inflammatory drugs (naproxen 500mg on demand).
During hospital stay, the symptoms of thyrotoxicosis subsided and biochemical euthyroidism was reached four weeks later. The remaining laboratory results such as haemoglobin and ESR also normalized, maintaining mild elevation of hepatic enzymes.
Discussion
Bearing in mind a woman in her fifties, with history of past PT and a recent contact with a relative with active PT, who reported vespertine fever, weight loss and cervical tumefaction, the main diagnostic hypotheses initially considered were tuberculosis and malignant neoplasms.
The examination of the patient was relatively benign, with the exception of an enlarged and tender thyroid, tachycardia and the absence of palpable neck lymph nodes or masses, adding hyperthyroidism to the possible differential diagnosis. The preliminary laboratorial results showed anaemia, ESR above 100mm/h, abnormal liver tests and confirmed elevated serum thyroid hormones levels. At this point, the additional workup was performed to study the thyroid and aetiology of hyperthyroidism and to exclude a malignant neoplasm (eventually with liver metastasis), considering that the common aetiologies of thyrotoxicosis wouldn’t explain these laboratory results.
The abdominal ultrasound and CT scan showed normal liver structure and the absence of nodules or lymph nodes enlargement, ruling out liver metastasis and abscesses. Other infectious entities associated with fever, constitutional symptoms and altered biochemical liver tests were also excluded. The thyroid ultrasonography was suggestive of subacute thyroiditis, a diagnosis which explained all the symptoms, signs and altered test results observed.
Although the diagnosis of subacute thyroiditis is fundamentally clinical4, it may be difficult to reach when presenting with atypical clinical manifestations5. In this case, the dominating symptom was not thyroid pain but rather fever and weight loss, leading us to focus our differential diagnosis on malignant and serious infectious illnesses. The laboratorial and imaging findings were crucial to establishing this diagnosis. All the laboratory alterations found were characteristic, namely the mild anaemia, CRP and ESR elevations6, elevated serum thyroid hormones levels and negative antithyroid antibodies. Liver enzymes are frequently elevated during the initial hyperthyroid phase3 and return to normal within one to two months. The specific cause of the cytocholestatic pattern is unknown but could be related to a viral infection or the hyperthyroidism itself. A radioiodine or technetium imaging study showing low to undetectable radionuclide uptake during the thyrotoxic phase helps confirm the diagnosis. In our case, the symptoms of thyrotoxicosis combined with typical laboratory, ultrasound alterations and clinical evolution were considered enough to establish the diagnosis of subacute thyroiditis, and the thyroid scintigraphy was deferred.
The management of these patients in the early stage is symptomatic pain relief and the control of hyperthyroidism symptoms7. Prednisolone can be considered as first line therapy for pain management in patients with severe pain and it can be associated with shorter disease duration7. As our patient had only mild cervical discomfort and the thyrotoxicosis symptoms subsided, this therapy was not needed. The characteristic course of this thyroiditis is, after the thyrotoxic phase, a rapid evolution through euthyroidism and then hypothyroidism, which lasts until thyroid follicle regeneration and hormone synthesis and secretion is resumed. As expected, our patient didn’t need specific treatment for hyperthyroidism. Periodic clinical and biochemical evaluations (every 6 weeks) are being performed, screening for the need for thyroid hormone supplementation when the hypothyroidism phase is reached.
Acknowledgments
We ackowledge Dr. Catarina Mira for the radiological diagnosis and related images, and Dr. Virgínia Visconti for english editing.
Figura I
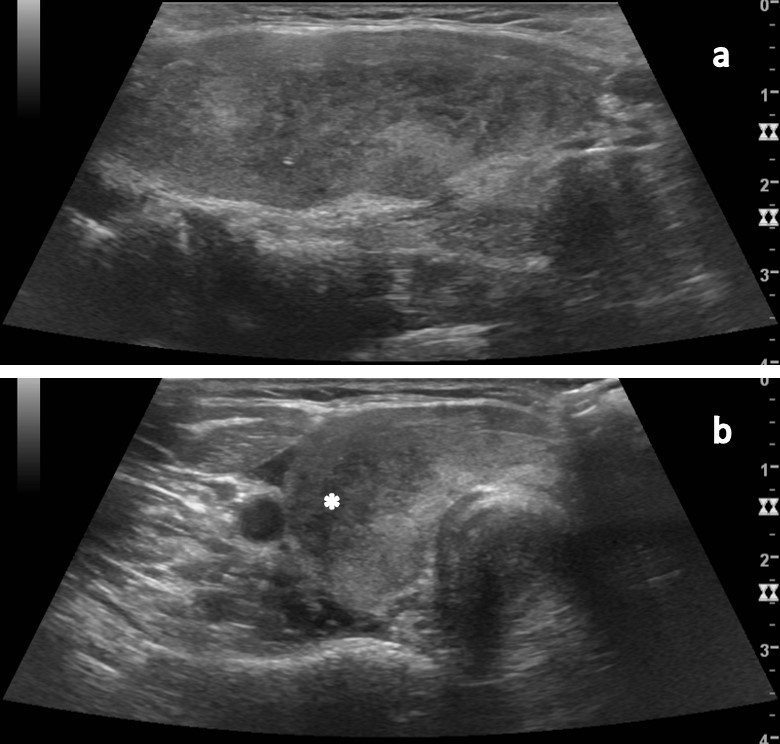
(a) Longitudinal view of right lobe shows diffuse heterogeneous echogenicity of the thyroid tissue. (b) Transverse view of right lobe shows poorly defined focal hypoechoic areas, non nodular, in bands (*), also present on the left lobe, in relation with the process of subacute/chronic thyroiditis.
BIBLIOGRAFIA
1. Taous A, Islam MS. Thyroiditis: differential diagnosis and management. Bangladesh J Otorhinolaryngol. 2010;16(1):48-53. doi: 10.3329/bjo.v16i1.5781.
2. Fatourechi V, Aniszewski JP, Fatourechi GZ, Atkinson EJ, Jacobsen SJ. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100. doi: 10.1210/jc.2002-021799.
3. Matsumoto Y, Amino N, Kubota S, Ikeda N, Morita S, Nishihara E, et al. Serial changes in liver function tests in patients with subacute thyroiditis. Thyroid. 2008;18:815-6. doi: 10.1089/thy.2007.0374.
4. Lazarus JH. Silent thyroiditis and subacute thyroiditis. In: Braverman LE, Utiger RD, editors. The Thyroid: A Fundamental and Clinical Text. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 1996. p.577.
5. Cunha BA, Chak A, Strollo S. Fever of unknown origin (FUO): de Quervain´s subacute thyroiditis with highly elevated ferritin levels mimicking temporal arteritis (TA). Heart Lung. 2010;39(1):73-7. doi: 10.1016/j.hrtlng.2009.06.006.
6. Pearce EN, Bogazzi F, Martino E, Brogioni S, Pardini E, Pellegrini G, et al. The prevalence of elevated serum C-reactive protein levels in inflammatory and noninflammatory thyroid disease. Thyroid. 2003;13(7):643-8. doi: 10.1089/105072503322239989.
7. Benbassat CA, Olchovsky D, Tsvetov G, Shimon I. Subacute thyroiditis: clinical characteristics and treatment outcome in fifty-six consecutive patients diagnosed between 1999 and 2005. J Endocrinol Invest. 2007;30:631-5. doi: 10.1007/BF03347442.