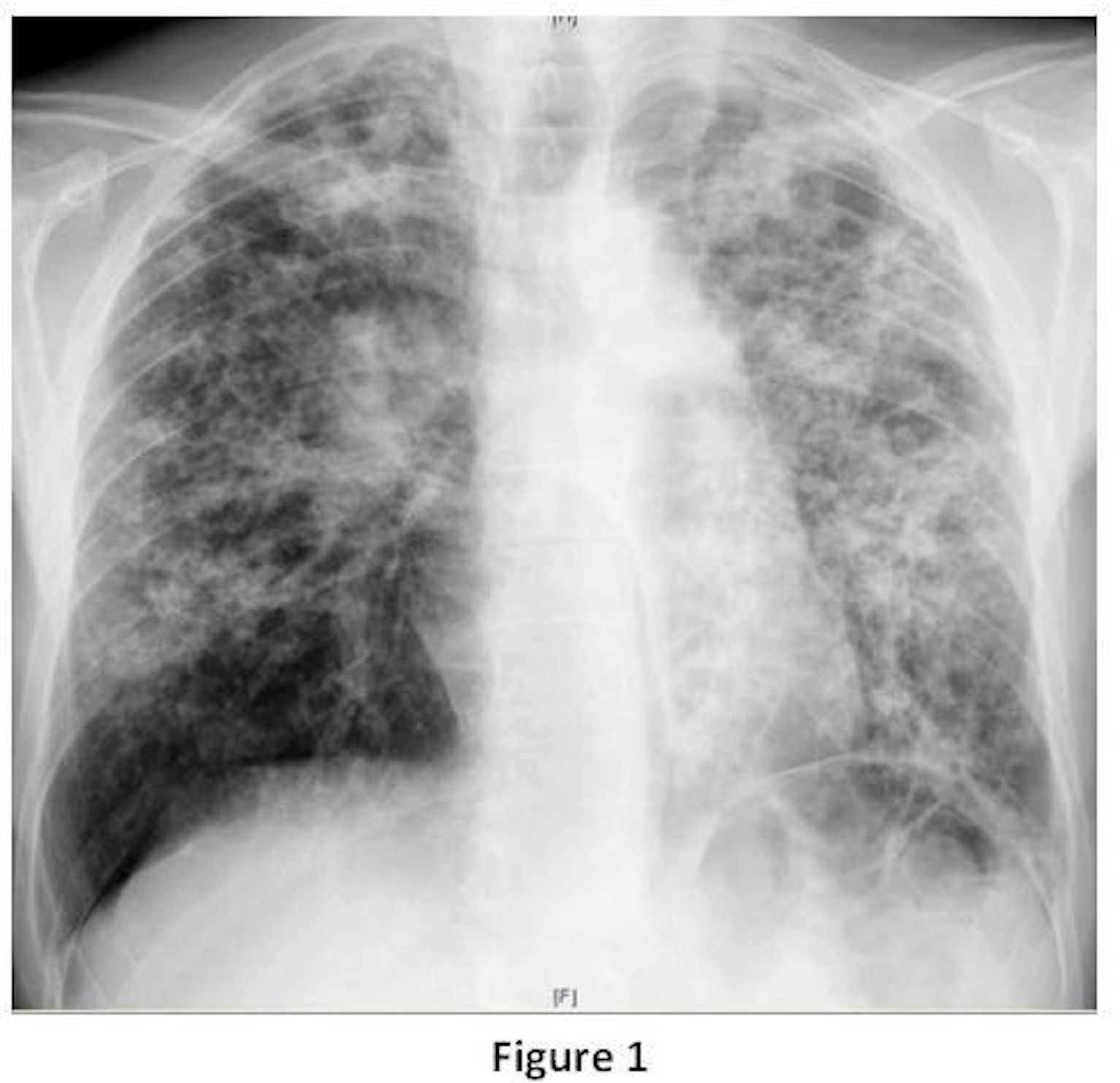
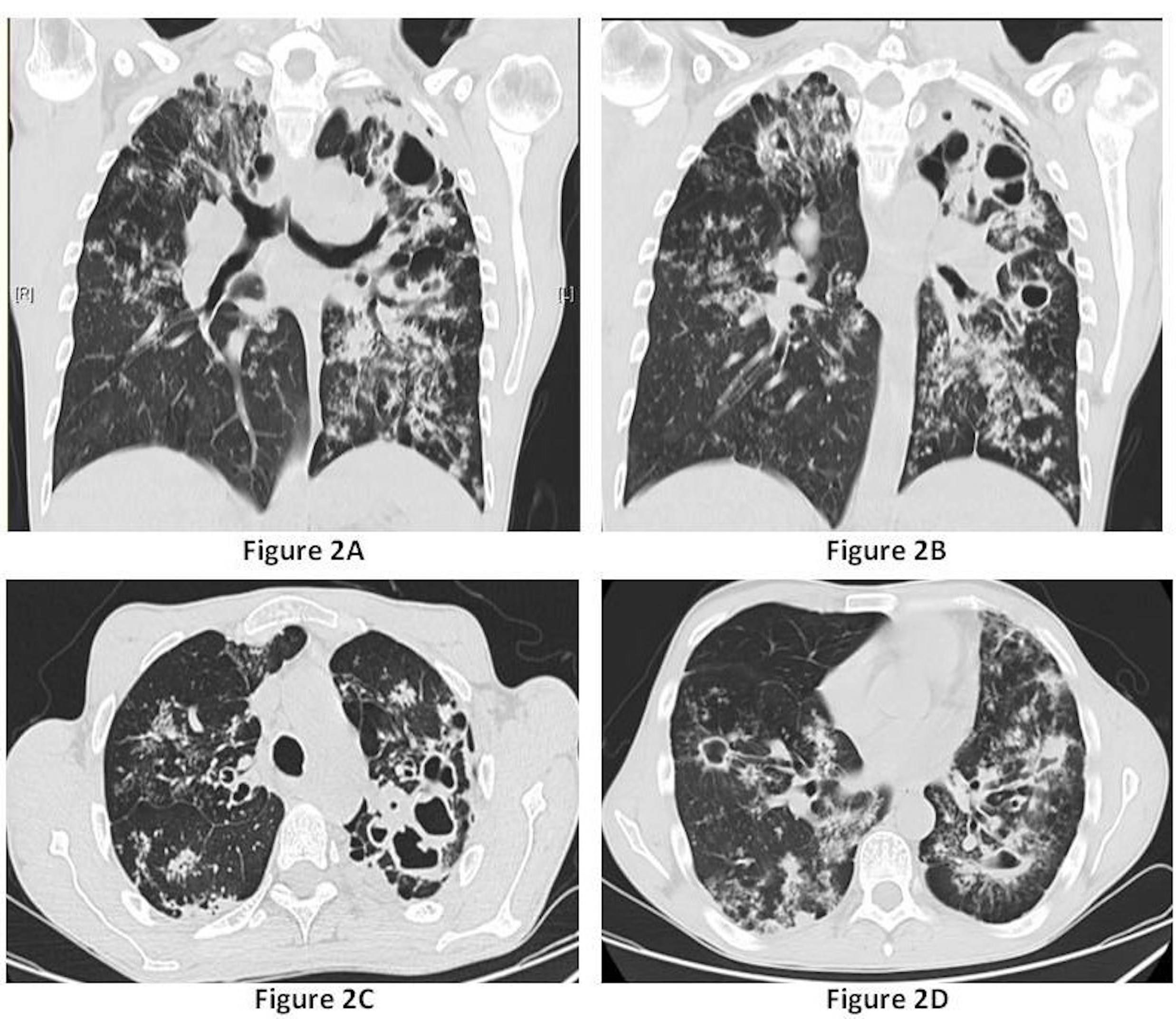
A 38-year-old man previously healthy with history of tobacco and drug use presented to the emergency department with persistent cough, fatigue, chest pain and weight loss. Denied fever, night sweats and hemoptysis. Physical exam was unremarkable. Routine laboratory studies showed mild elevation of inflammation markers and hypochromic microcytic anemia. Electrocardiogram was normal sinus rhythm, and arterial blood gas analysis revealed a mild hypoxemia (pO2 71mmHg). Chest radiograph (Fig. 1) exhibited extensive bilateral perihilar, mid and upper zones ill-defined consolidations with concomitant variable-sized cavities with irregular wall thickening. And chest CT scan (lung window) confirmed the extensive airspace consolidations and irregular thick-walled cavity formation in the posterior segments of the upper lobes (Fig. 2C) and superior segments of the lower lobes (Fig. 2D); left upper lobe (Fig. 2A) and right mid and upper lobes (Fig. 2B). Bronchiectasis and tree-in-bud opacities are seen in the left upper and lower lobes (Fig. 2A-D) consistent with endobronchial spread of disease.HIV was negative. Acid-fast bacilli smear and mycobacterium culture of a stained sputum were positive. Gene Xpert assay for M. tuberculosis was positive with the susceptibility testing for rifampin. Patient significantly improved with first-line agents anti-tuberculous therapy, maintaining follow-up in outpatient department.
Tuberculosis is currently the world´s second leading infectious cause of death, and one-third of the world´s population has been infected by tuberculosis.1 One microorganism, Mycobacterium tuberculosis, causes human tuberculosis in nearly all cases, transmitted from person to person through inhalation of droplets containing tubercle bacilli. The risk for tuberculosis transmission increases when source patients have airway and cavitary disease.2 The radiologic features associated with primary and post-primary (or reactivation) tuberculosis correlate best with the host immune status than with the time elapsed since initial infection.3 Conventional mycobacterium culture remains the most sensitive test for detection of tuberculosis.2
Figura I
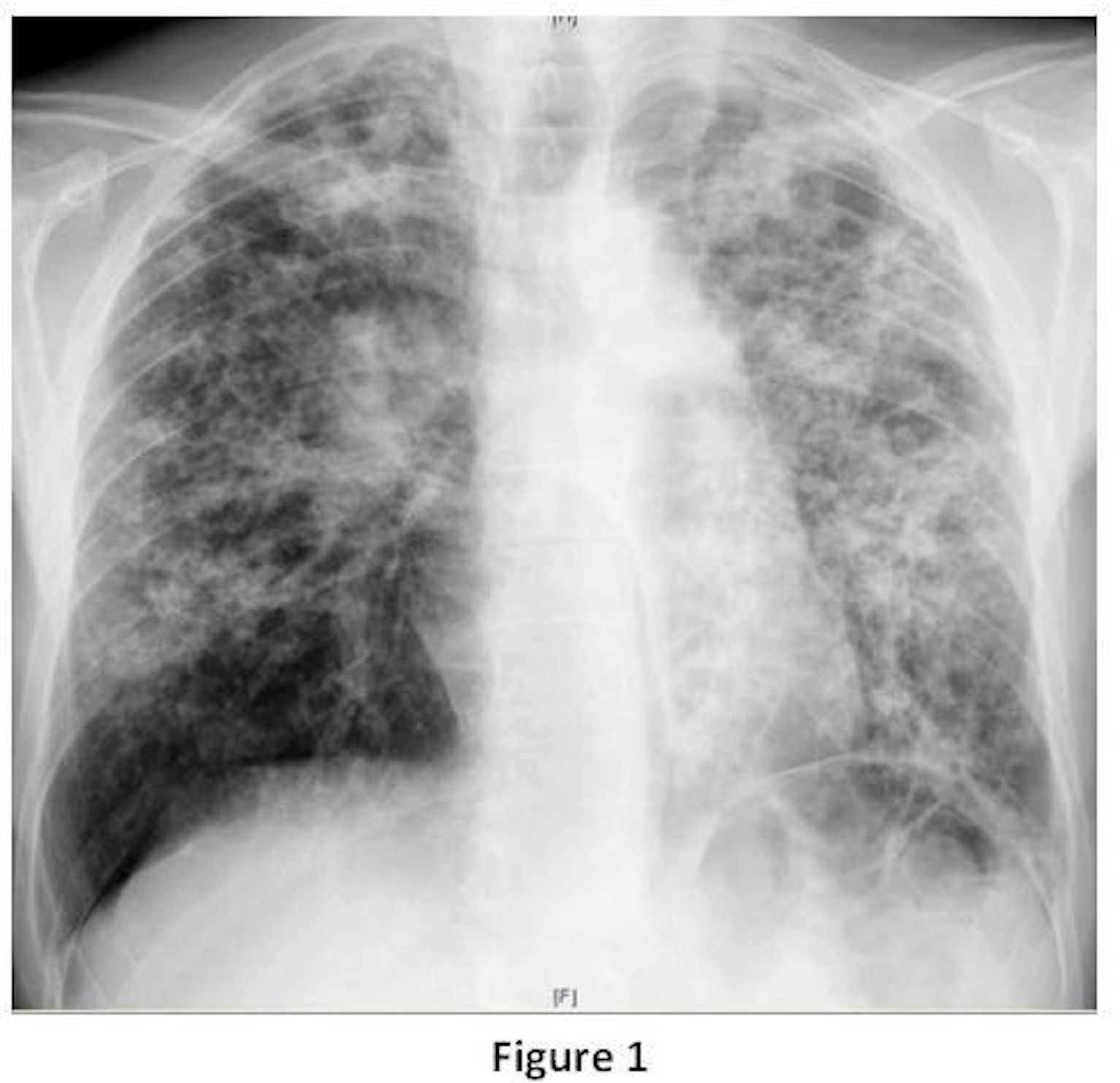
Chest radiograph exhibited extensive bilateral consolidations with cavities.
Figura II
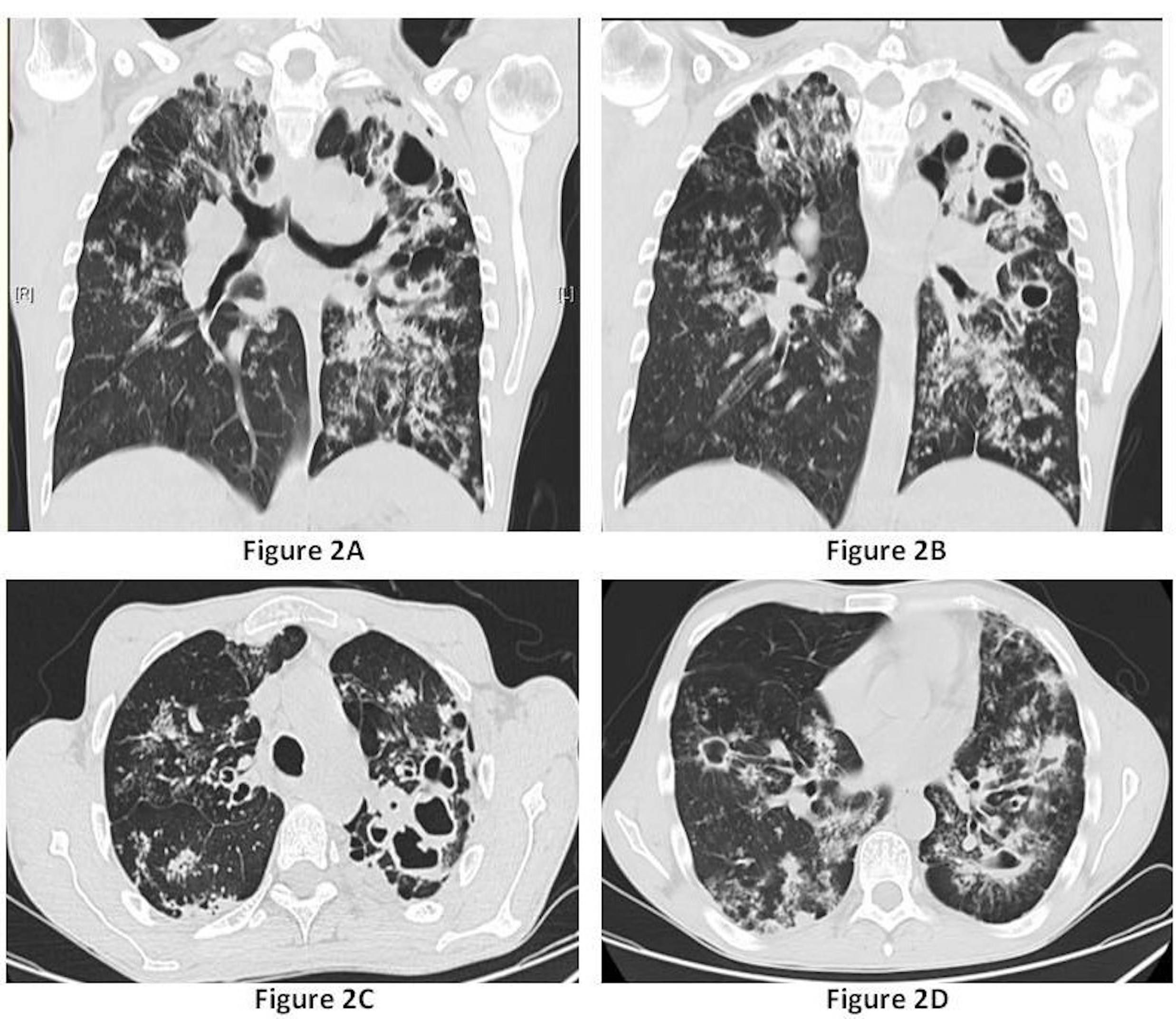
Coned-down coronal (Fig. 2A and 2B) and axial (Fig. 2C and 2D) contrast-enhanced chest CT (lung windows).
BIBLIOGRAFIA
1. Sulis G, Roggi A, Matteelli A, et al: Tuberculosis: epidemology and control. Mediterr JHematol Infect Dis. 2014; 6(1):e2014070.
2. World Health Organization. Global tuberculosis report 2018. WHO/CDS/TB/2018.20.
3. Nachiappan AC, Kasra R, Shi X, et al: Pulmonary Tuberculosis: Role of Radiology inDiagnosis and Management. RadioGraphics 2017; 37:52–72.