Introduction: Fahr’s syndrome (FS) is a disorder characterized by bilateral and symmetrical calcifications over the basal ganglia, dentate nucleus and cerebral cortex1-4. When primary familiar brain calcification is present, the term used is Fahr’s disease, with FS reserved for secondary causes3. The etiology of FS is poorly understood; it has been associated mostly with disorders of calcium and phosphorus metabolism, but can also be associated with infectious, metabolic and genetic diseases2, 4, 5.
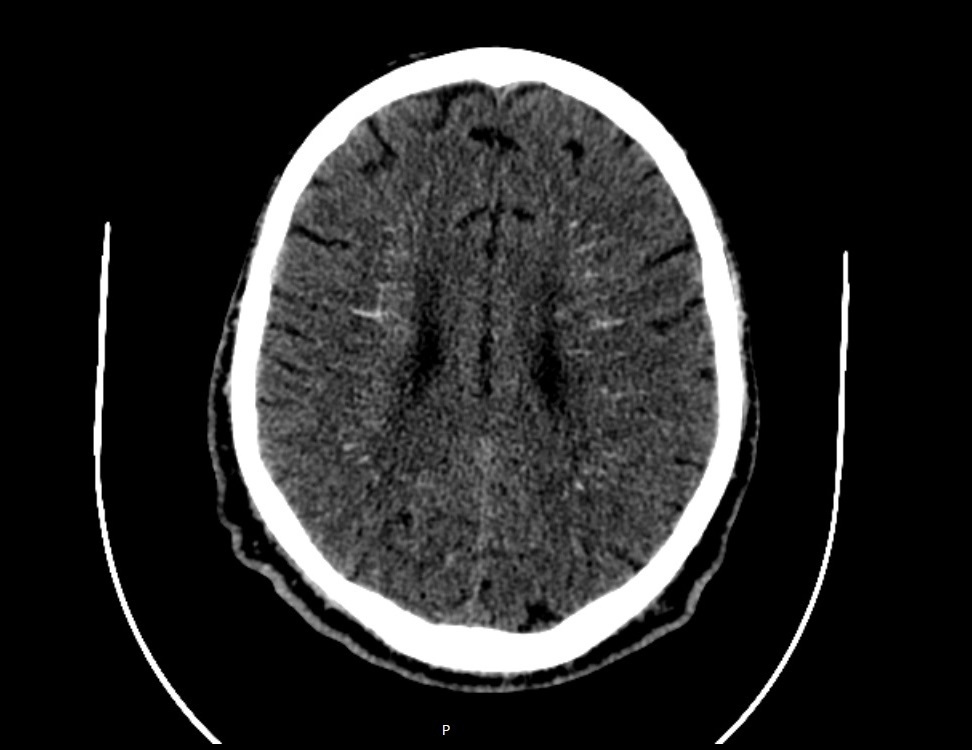
Case report: A 71-year-old male patient was admitted to the Emergency Room due to a symptomatic first seizure. Medical history was unremarkable. He had no past history of epilepsy, neck radiation or thyroid surgery. Family history was irrelevant. Laboratory investigations revealed normal renal and thyroid function, hypocalcaemia of 6.2 mg/dL (normal range 8.4-9.7), hyperphosphatemia of 6.1 mg/dL (normal range 2.7-4.5), normal serum albumin of 4.2 g/dL (reference range 3.4-4.8), low 25-OH vitamin D levels of 50 nmol/L (normal range 62.5-200), normal magnesium of 1.57 (normal range 1.3-2.1), low calciuria of 16 mg/24h (normal range 100-320) and undetectable PTH <5.0 pg/mL (reference range 15.0-65.0). Computed tomography scan of the brain revealed multiple calcifications involving the basal ganglia (Figure 1 and Figure 2). Based on clinical, analytical and radiological findings, the patient was diagnosed with primary hypoparathyroidism and the diagnosis of FS was assumed.
Conclusion: We report a case of FS with basal ganglia calcification in a patient with primary hypoparathyroidism that first presented with seizures. Reduced PTH causes hypocalcaemia and hyperphosphatemia that promotes brain calcification4. Although rare, this syndrome should be suspected when symmetrical calcification of basal ganglia is seen. The most common reported metabolic disorders that cause FS are hypoparathyroidism and pseudohypoparathyroidism4. If no cause for primary brain calcification is detected, the diagnosis of primary familial basal calcification should be considered and genetic testing is recommended4.
Figura I

Computed tomography, transversal plan, showing multiple, symmetric calcifications in the basal ganglia
Figura II
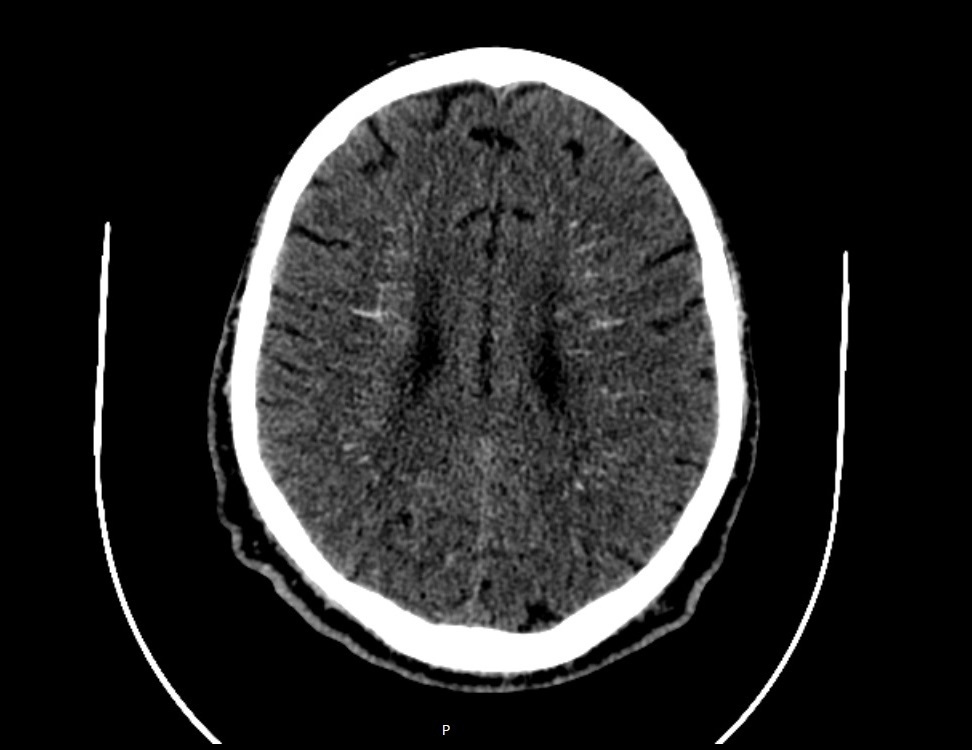
Computed tomography, transversal plan, showing multiple, symmetric calcifications in the basal ganglia
BIBLIOGRAFIA
1 T. Benke, E. Karner, K. Seppi, M. Delazer, J. Marksteiner, and E. Donnemiller, ´ Subacute Dementia and Imaging Correlates in a Case of Fahr ´ s Disease ´, J Neurol Neurosurg Psychiatry, 75 (2004), 1163-5.
2 K. Jaworski, M. Styczynska, M. Mandecka, J. Walecki, and D. A. Kosior, ´ Fahr Syndrome - an Important Piece of a Puzzle in the Differential Diagnosis of Many Diseases ´, Pol J Radiol, 82 (2017), 490-93.
3 Y. J. Lee, S. Park, Y. W. Kim, K. M. Park, I. H. Kim, J. H. Park, and B. S. Park, ´ A Case of Seizure Revealing Fahr ´ s Syndrome with Primary Hypoparathyroidism ´, Am J Case Rep, 19 (2018), 1430-33.
4 S. Saleem, H. M. Aslam, M. Anwar, S. Anwar, M. Saleem, A. Saleem, and M. A. Rehmani, ´ Fahr´s Syndrome: Literature Review of Current Evidence ´, Orphanet J Rare Dis, 8 (2013), 156.
5 A. Swami, and G. Kar, ´ Intracranial Hemorrhage Revealing Pseudohypoparathyroidism as a Cause of Fahr Syndrome ´, Case Rep Neurol Med, 2011 (2011), 407567.