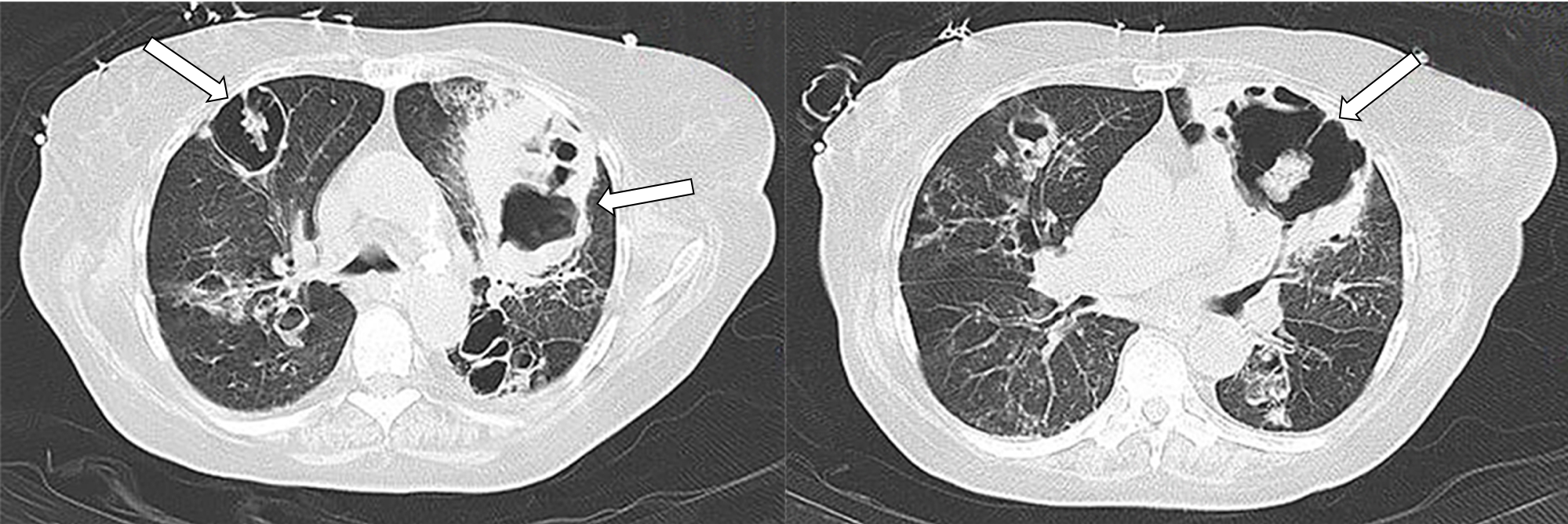
A 74-year-old woman, diabetic, hypertensive and active smoker with bronchiectasis, presented to the emergency department (ED) with cough and dyspnea for 3 days. She was hypoxemic and had elevated inflammatory parameters and a chest X Ray with a left lung consolidation. The patient was admitted with the diagnosis of community acquired pneumonia and acute respiratory failure. The development of hypotension and a severe hypoxemia (PaO2/FiO2 ratio of 156) prompted transfer to an Intensive Care Unit (ICU) for invasive mechanical ventilation. She presented hemoptysis. A bronchoscopy and a chest computed tomography were preformed, disclosing lung lesions with a halo, very suggestive of invasive pulmonary aspergillosis (IPA) (Figure 1). Galactomannan antigen was detected in bronchoalveolar lavage. Treatment with Voriconazole was initiated but despite that death was the outcome.
IPA is an opportunistic life-threatening infection occurring mainly in severely immunocompromised patients but recently it has been described in immunocompetent ICU patients.1,2 It may occur in patients with combined lung immune imbalance with systemic intrinsic and corticoid-induced immune dysfunctions, such as patients with underlying lung disease and also in patients with systemic illness.1,3 Some reports also described IPA in patients on mechanical ventilation.1 IPA is characterized by pulmonary parenchyma invasion with vascular erosion and necrosis that is caused by opportunistic fungi of theAspergillus species.3 Due to its difficult diagnosis and treatment delay, IPA has an high mortality rate.1ľ4 In chronic obstructive lung disease mortality range from 70 to 95% and in patients in ICU may exceed 80%.2,3 Therefore early diagnosis and treatment are crucial. Despite some limitations, the conventional microbiological methods, imaging and non-culture-based tests remain the diagnostic cornerstone of IPA. While not exclusive, the IPA is the most common cause of halo signal in a population at high risk for fungal infection.4
Figura I
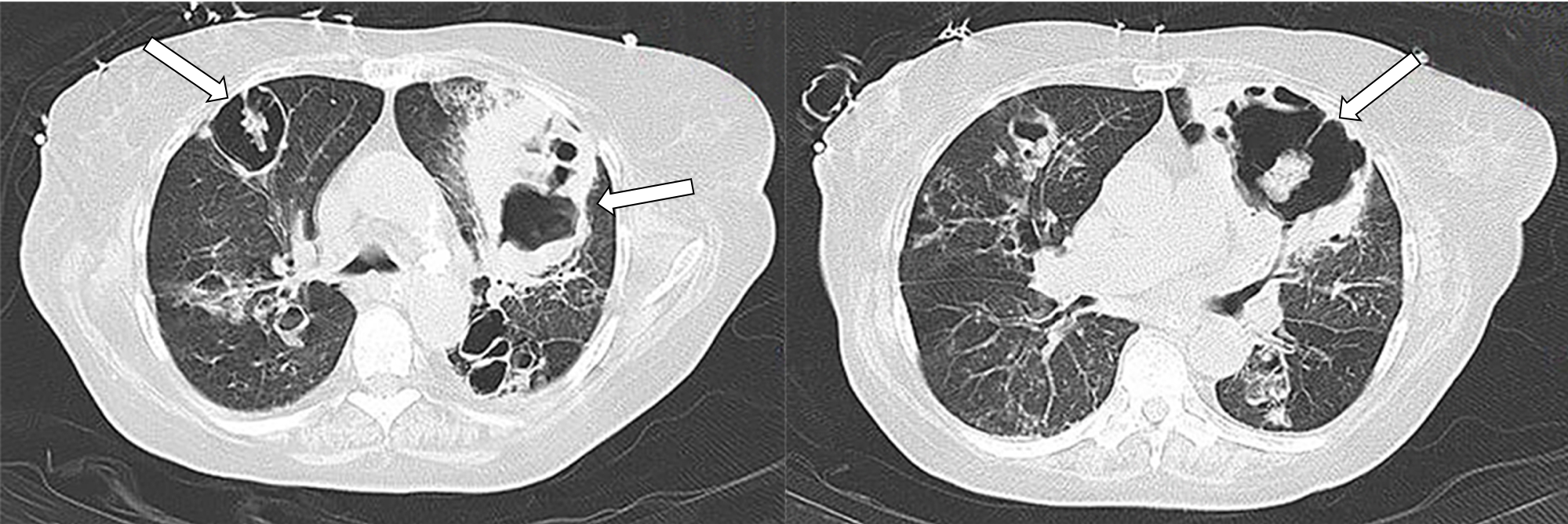
Chest computed tomography showing the characteristic pulmonary lesions suggestive of IPA.
BIBLIOGRAFIA
1. Charles M V P, Joseph N M, Easow J M & Ravishankar M. Invasive Invasive pulmonary aspergillosis caused by aspergillus versicolor in a patient on mechanical ventilation. Australas. Med. J. 4, 632ľ634 (2011).
2. Basseti M, Righi E, De Pascale G, De Gaudio R, Giarratano A, Mazzei T et al. How to manage aspergillosis in non-neutropenic intensive care unit patients. Crit. Care 18, 1ľ12 (2014).
3. Ader F, Bienvenu A, Rammaert B & Nseir S. Management of invasive aspergillosis in patients with COPD: rational use of voriconazole. Int. J. Chron. Obstruct. Pulmon. Dis. 279 (2009).
4. Moura S, Cerqueira L & Almeida A. Invasive pulmonary aspergillosis: current diagnostic methodologies and a new molecular approach. Eur. J. Clin. Microbiol. Infect. Dis. 37, 1393ľ1403 (2018).