Introduction
IgA dominant acute post-infectious glomerulonephritis (APIGN) is a rare morphologic variant of acute post-infectious glomerulonephritis (GN) described in the last decade. It is a challenging diagnosis and usually appears during or after aStaphylococcusinfection.1 This clinical entity is more prevalent in males, older than 60 years with diabetes mellitus, frequently superimposed on diabetic kidney disease. Other risk factors for this entity are neoplastic disease, intravenous drug or alcohol abuse.2–5Staphylococcusinfections have increasing importance in medicine, given their rising prevalence and resistance to antibiotics.
We present the case of a patient diagnosed with IgA dominant APIGN, after an infectious endocarditis due to methicillin-susceptibleStaphylococcus aureus(MSSA).
Case description
70 year-old male, with history of hypertension and type 2 diabetes mellitus (with good metabolic control but with suspected diabetic kidney disease), presented to emergency room with vomits, malaise and fever (tympanic temperature 39.2ºC). Physical examination revealed an aortic systolic murmur III/VI, precarious oral hygiene and edentulism. Blood tests revealed leukocytosis (18.20x109/L) with neutrophilia (16.80x109/L), serum creatinine 1.20mg/dL and C-reactive protein 3.93mg/dL. Blood cultures and urine culture were performed and amoxicillin/clavulanic acid was initiated. Patient was admitted into a ward.
Three days after admission, MSSA was isolated in blood cultures and antibiotics were adjusted to flucloxacillin and gentamycin. After transesophageal echocardiogram revealed a vegetation on a native bicuspid aortic valve, infectious endocarditis was diagnosed, given that 2 major Duke criteria for endocarditis were fulfilled. Gentamycin was later discontinued since it was a MSSA endocarditis.
On the 13thday of antibiotic therapy, the patient showed deterioration of renal function, with maximum serum creatinine 4.70 mg/dL, despite discontinuation of all potential nephrotoxic drugs with worsen hypertension control and development of peripheric edema.
Urine sample revealed microscopic hematuria and proteinuria of 1925mg/24h. HIV, HBV and HCV serologies were negative. Anti ds-DNA, ANA’s, ANCA’s and anti-glomerular basement membrane antibody were negative. Anti-Streptolysin levels were within normal range. C3 and C4 level were normal. Immunoglobulin levels were normal.
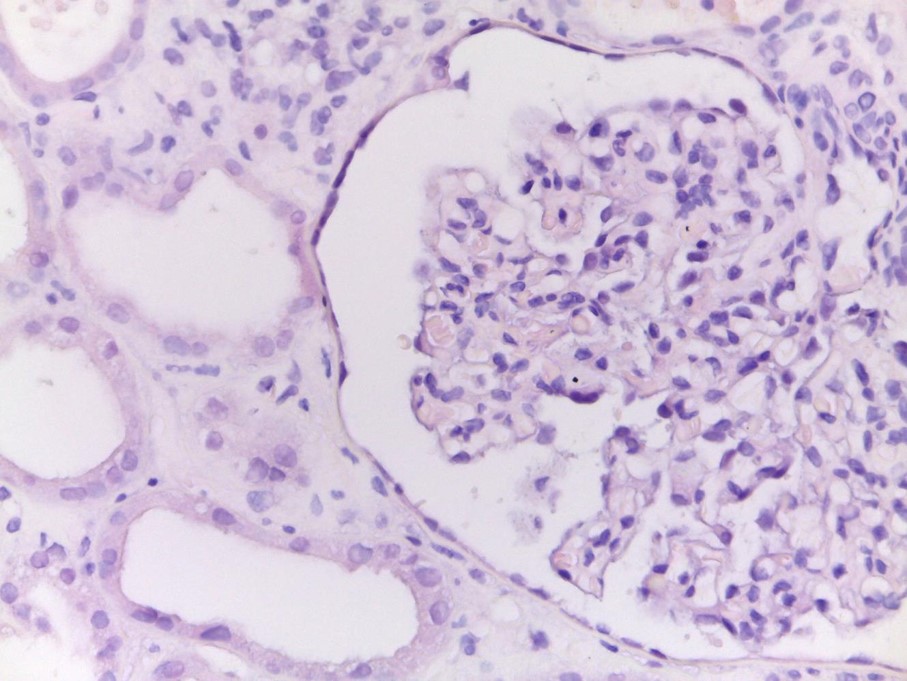
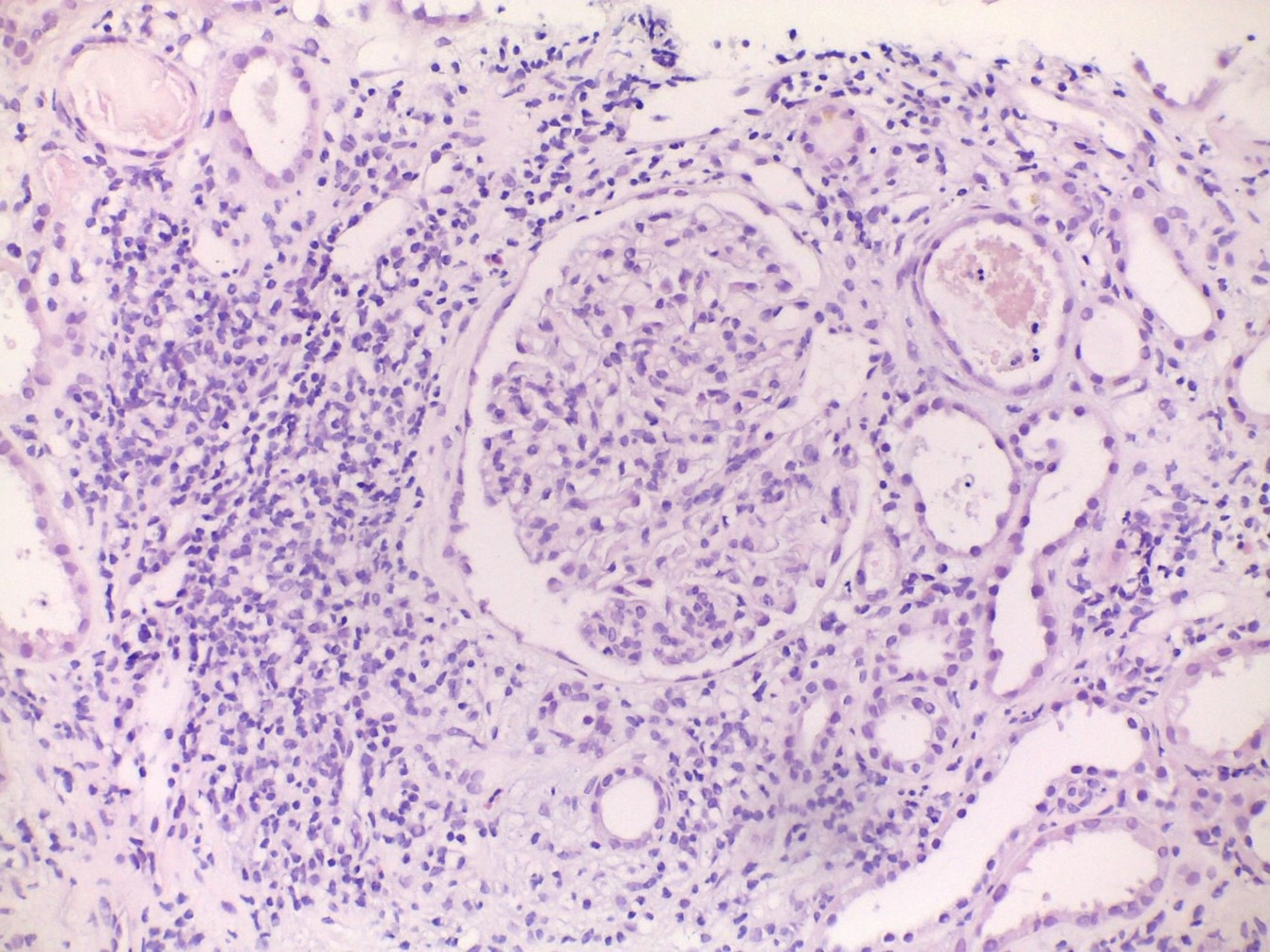
Renal biopsy was performed and revealed glomeruli with mild mesangial and moderate endocapillary hypercellularity (Fig. 1), with crescents, mild tubular atrophy and interstitial fibrosis and acute interstitial nephritis with eosinophils (Fig. 2). Immunofluorescence showed dominant IgA and C3 deposition with fine granular deposits with mesangial dominance. Staining for IgG, IgM, fibrinogen, C1q, κ and λ chains was negative. Electron microscopy was not performed. Proliferative GN with IgA and C3 deposits was diagnosed, compatible with IgA dominant APIGN. The biopsy also revealed acute interstitial nephritis due to nephrotoxicity.
INSERT FIGURE 1….
INSERT FIGURE 2….
Patient was discharged after completing 4 weeks of flucloxacillin, referred to the Nephrology out-patient clinic. After one year of follow-up he had returned to his basal renal function and proteinuria and microscopic hematuria disappeared.
Discussion
IgA dominant APIGN is an immune complex-mediated acute GN. APIGN associated with staphylococcal infections was first described by Koyama et al. in 1995 in a series of 10 patients. At the time, it was described as a GN associated with methicillin-resistant Staphylococcus aureus.6 Later in 2003, Nasr et al., published a review of APIGN biopsies where he described 5 biopsies with IgA-dominant glomerular deposits in patients who had staphylococcal infections documented. In this article they introduced the term IgA dominant APIGN.3
Patients usually present with acute kidney injury, microscopic haematuria and variable proteinuria (often in nephrotic range), frequently during an ongoing staphylococcal infection, as it happened in the presented case.2,5,7,8
Most frequent sites of infection are the skin, deep-seated abscesses, lung, joints and heart infections.1,2,5,9 Risk factors associated with this disease are elderly (>60 years), male sex, diabetes mellitus, diabetic kidney disease, neoplastic disease, intravenous drug or alcohol abuse.2–5 Our patient had some of these characteristics - he was an elderly diabetic patient with diabetic kidney disease and was diagnosed with infectious endocarditis.
Pathogenic mechanisms are still poorly understood, butStaphylococcus aureusenterotoxins (B and C) acting as superantigens are thought to play a major role by inducing massive cell activation and proinflammatory cytokines release. This leads to polyclonal activation of IgA and IgG, resulting in immune complex formation and glomerular deposition.1,2,6,7,10
Histologically, there are some variable light microscope findings, including endocapillary proliferative GN (most frequent subtype), mesangial proliferative GN, diffuse (both mesangial and endocapillary) proliferative GN, crescentic or necrosis GN. In acute phase, inflammation can be present with numerous infiltrating neutrophils. During subacute phase fewer neutrophils are usually present compared with acute phase. Glomerular IgA deposits with granular pattern on immunofluorescence, resembling IgA nephropathy, are frequent and usually IgA is the dominant or co-dominant (with IgG) class of immune complex deposited. Co-deposition of C3 is also frequently seen. Subepithelial hump-shaped electron dense deposits are unusual, but very suggestive of this entity.5–7,11,12 Our patient presented with moderate endocapillary proliferative GN, acute interstitial nephritis with eosinophils presence and dominant IgA and C3 deposition with fine granular deposits with mesangial dominance in immunofluorescence. These findings suggested a subacute course of the disease, as well as some degree of acute interstitial nephritis due to nephrotoxicity.
The diagnosis can be challenging, since there is a large range of differential diagnosis: IgA nephropathy, IgA vasculitis, other immune complex GN, ANCA vasculitis.2,4 Nephrotoxicity cannot be ruled out without performing kidney biopsy. Due to this possible etiology, we suspended all potential nephrotoxic drugs, namely gentamycin, when the patient presented acute kidney injury.
The distinction between IgA dominant APIGN and IgA nephropathy is extremely important, due to their different prognosis and treatment. IgA nephropathy usually affects younger patients and tends to follow a more protracted course of the nephritic or even nephrotic syndrome, but hypocomplementemia is rarely present.2,7,9 Renal biopsy findings alone cannot exclude IgA nephropathy, since both entities can reveal mesangial hypercellularity with IgA and C3 immune complex deposits. However, clinical findings and history of staphylococcal infection with rapid progression of kidney injury point towards IgA dominant APIGN, rather than IgA nephropathy.2
Treatment of IgA dominant APIGN is based on antibiotic therapy for underlying infection. The role of steroids is highly controversial and should only be considered if renal disease continues to progress despite adequate antibiotic therapy and infection control.2,9,11,12 In our case we chose to maintain the flucloxacillin scheme due to its efficacy against MSSA and low nephrotoxicity potential.
Prognosis of IgA dominant APIGN is generally guarded with varying outcomes described in different series. Full recovery of renal function has been described in 16-55%, partial recovery in 12-49% and progression to end-stage kidney disease in 20-41%, according to different series.2,5,7,11 Poor prognosis is frequently associated with older age, diabetes mellitus, tubulointerstitial scarring and presence of underlying kidney disease (frequently diabetic kidney disease).2,5,11 Although our patient had multiple risk factors for poor outcome, he was able to fully recover his basal renal function. The fact that our patient presented with moderate (rather than severe) endocapillary proliferation and had a contribute of the acute interstitial nephritis (most likely due to gentamycin) are two possible justifications for the better outcome of our patient.
IgA dominant APIGN is a rare disease, with increasing incidence worldwide, due to the increasing prevalence of diabetes mellitus and ageing population. In older, diabetic patients being treated for staphylococcal infection who presents with rapidly worsening kidney injury one should always suspect of this entity.
Acknowledgements
The authors would like to thank to PhD Vitor Sousa for the contribution with the histology images and respective descriptions.
Patient informed consent
Obtained.
Conflicts of Interests
The authors declare there are no competing interests.
Figura I
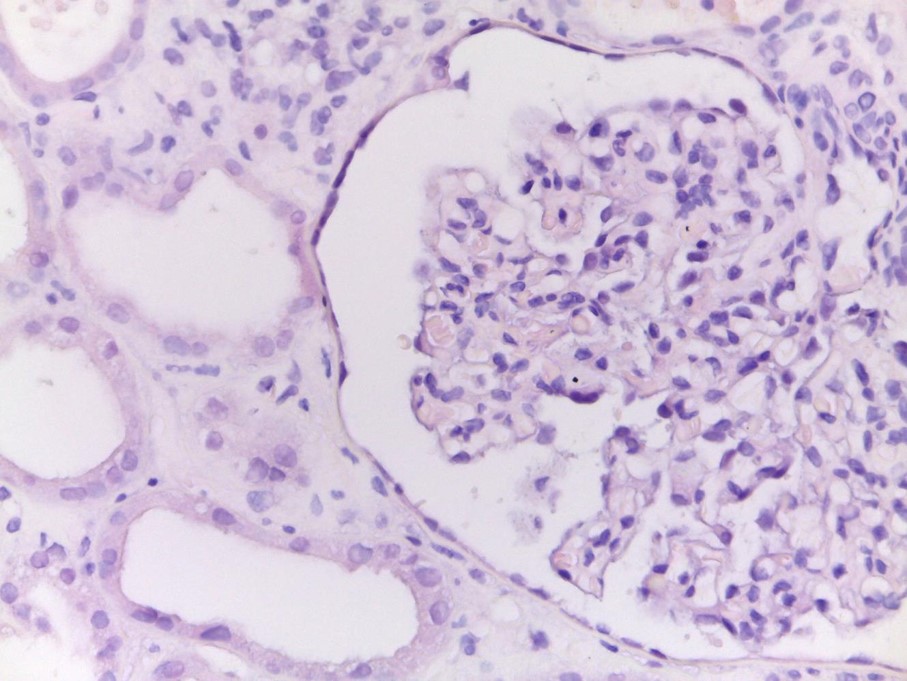
Renal biopsy revealing glomeruli with mild mesangial and moderate endocapillary hypercellularity (figure 1) (H&E x400).
Figura II
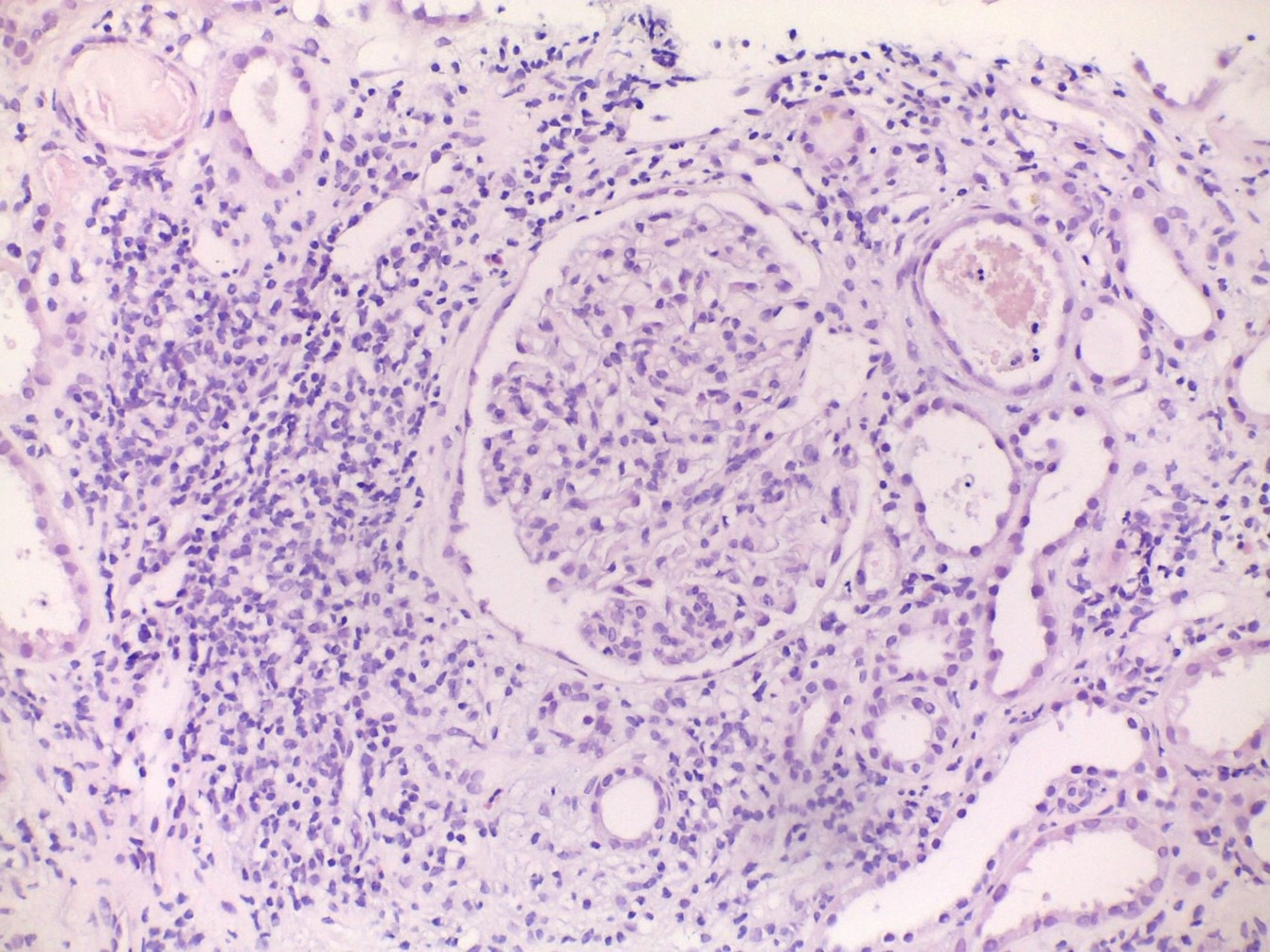
Renal biopsy revealing tubular atrophy, interstitial fibrosis and acute interstitial nephritis (H&E x200).
BIBLIOGRAFIA
1. Wehbe E, Salem C, Simon JF, Navaneethan SD, Pohl M. IgA-dominant Staphylococcus infection-associated glomerulonephritis: case reports and review of the literature. NDT Plus. 2011 Jun;4(3):181–5.
2. A. Hemminger J, A. Satoskar A. Staphylococcus Infection-Associated Glomerulonephritis. In: Bacterial Infections and the Kidney. 2017. p. 37–61.
3. Nasr SH, Markowitz GS, Whelan JD, Albanese JJ, Rosen RM, Fein DA, et al. IgA-dominant acute poststaphylococcal glomerulonephritis complicating diabetic nephropathy. Hum Pathol. 2003 Dec;34(12):1235–41.
4. Satoskar AA, Suleiman S, Ayoub I, Hemminger J, Parikh S, Brodsky SV, et al. Staphylococcus Infection–Associated GN – Spectrum of IgA Staining and Prevalence of ANCA in a Single-Center Cohort. Clin J Am Soc Nephrol. 2017 Jan 6;12(1):39–49.
5. Bu R, Li Q, Duan Z, Wu J, Chen P, Chen X, et al. Clinicopathologic Features of IgA-Dominant Infection-Associated Glomerulonephritis: A Pooled Analysis of 78 Cases. Am J Nephrol. 2015;41(2):98–106.
6. Koyama A, Kobayashi M, Yamaguchi N, Yamagata K, Takano K, Nakajima M, et al. Glomerulonephritis associated with MRSA infection: A possible role of bacterial superantigen. Kidney Int. 1995 Jan;47(1):207–16.
7. Gaut JP, Mueller S, Liapis H. IgA dominant post-infectious glomerulonephritis update: pathology spectrum and disease mechanisms. Diagn Histopathol. 2017 Mar;23(3):126–32.
8. Shimamura Y, Maeda T, Gocho Y, Ogawa Y, Takizawa H. IgA-dominant infection-related glomerulonephritis. Nefrol Publicacion Of Soc Espanola Nefrol. 2018 Mar 26;
9. Caetano J, Pereira F, Oliveira S, Alves JD. IgA-dominant postinfectious glomerulonephritis induced by methicillin-sensitive Staphylococcus aureus. BMJ Case Rep. 2015 May 14;2015:bcr2014208513.
10. Koyama A, Sharmin S, Sakurai H, Shimizu Y, Hirayama K, Usui J, et al. Staphylococcus aureus cell envelope antigen is a new candidate for the induction of IgA nephropathy. Kidney Int. 2004 Jul;66(1):121–32.
11. Nasr SH, D’Agati VD. IgA-Dominant Postinfectious Glomerulonephritis: A New Twist on an Old Disease. Nephron Clin Pract. 2011;119(1):c18–26.
12. Satoskar AA, Nadasdy G, Plaza JA, Sedmak D, Shidham G, Hebert L, et al. Staphylococcus infection-associated glomerulonephritis mimicking IgA nephropathy. Clin J Am Soc Nephrol CJASN. 2006 Nov;1(6):1179–86