A 40-year-old man was admitted in the emergency department with a 15-day history of fever, dyspnea and dry cough. On evaluation he had significant hypoxemia and the chest radiograph showed diffuse interstitial bilateral lung infiltrates. He tested positive for the human immunodeficiency virus (HIV) 1 and bronchoalveolar lavage analysis revealed a positive direct fluorescent antibody staining for Pneumocystis jirovecii, confirming the diagnosis of Pneumocystis jirovecii pneumonia (PJP), for which he started treatment with trimethoprim-sulfamethoxazole (TMP/SMX) and prednisolone.
The patient evolved with persistent hypoxemia, high fevers and progressive pulmonary infiltrates. At this point, the 10thday of hospitalization, we changed the treatment to primaquine plus clindamycin, assuming a possible failure of TMP/SMX.
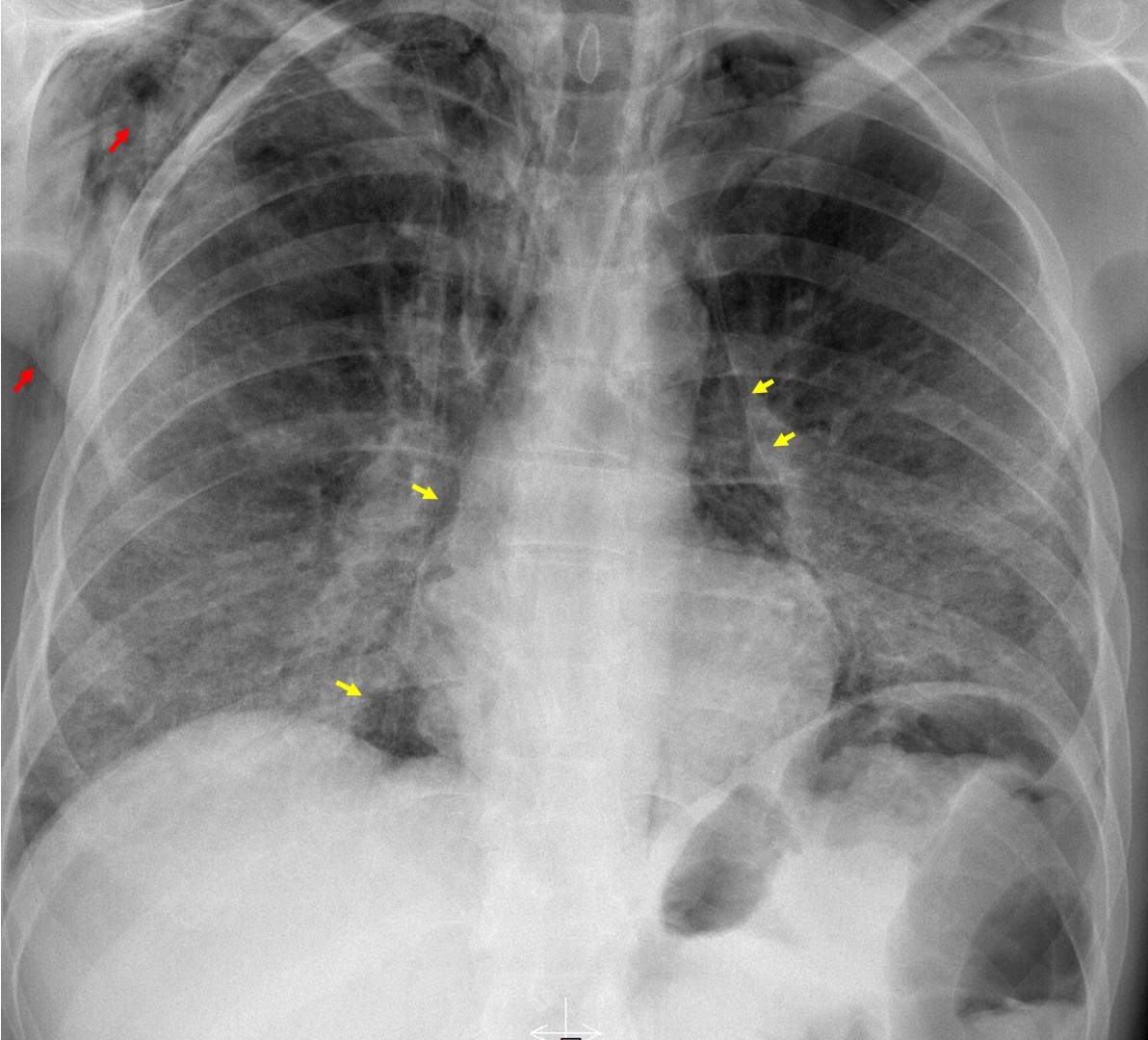
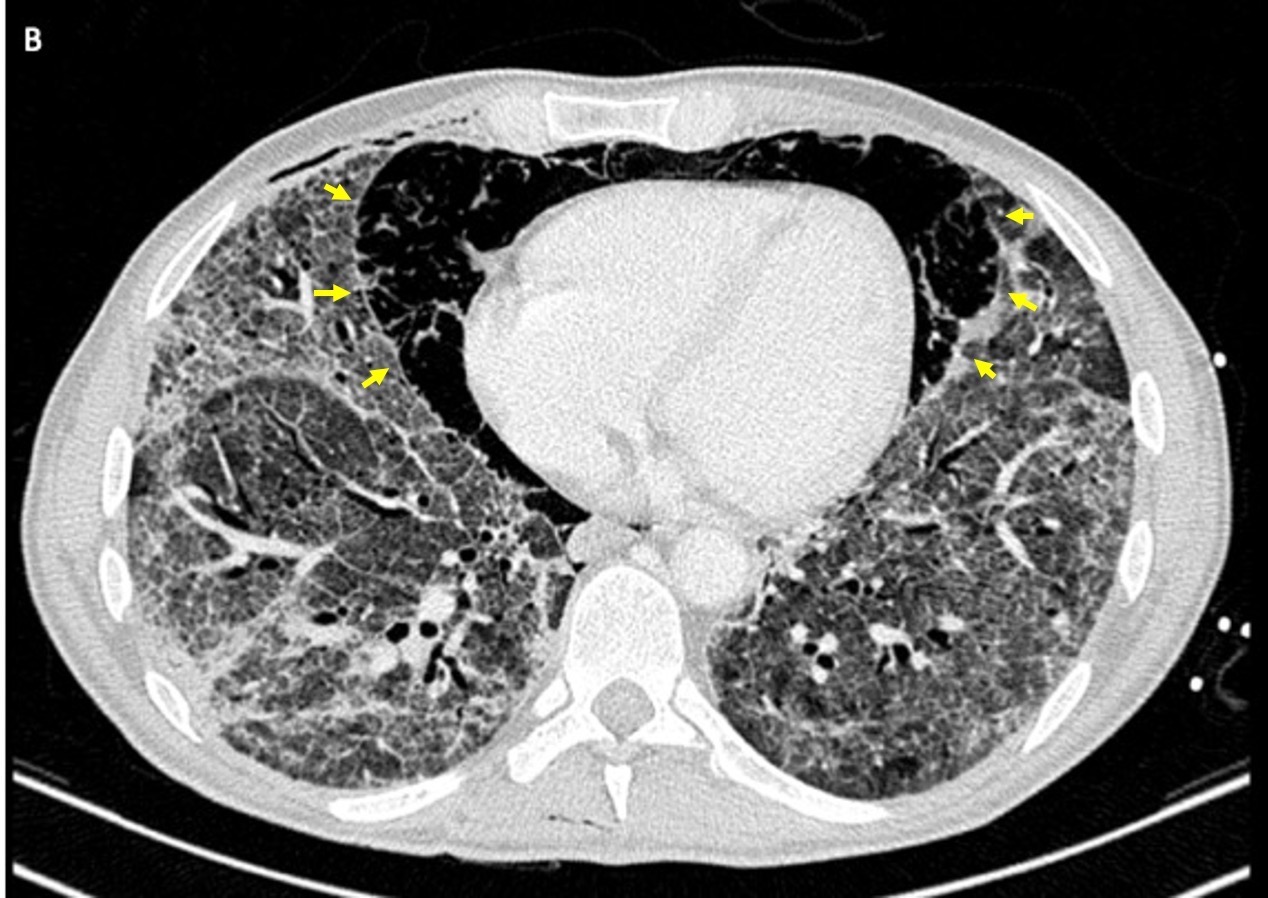
On the 14thday of hospitalization he complained of chest tightness and had an acute deterioration in his oxygen saturation. Physical examination revealed swelling and crepitus of the neck and thorax and the chest radiograph (Fig. 1) showed a thin radiolucent line delineating mediastinal air that outlined the lateral borders of the heart and that extended superiorly along the trachea, compatible with pneumomediastinum, as well as subcutaneous emphysema. Computed tomography (Fig. 2) confirmed the presence of an exuberant pneumomediastinum, and showed diffuse and extensive bilateral ground-glass opacities and cystic lung lesions.
The patient required mechanical ventilation, which exacerbated the pneumomediastinum with progression into a tension pneumomediastinum with hemodynamic instability, for which a subxiphoid mediastinal drain was emergently placed. Despite treatment, the patient’s condition continued to decline and he died on the 30thday of hospitalization.
Pneumomediastinum is a rare complication of PJP, with an incidence between 0.4% and 3.3%, and is more frequent in HIV positive patients.1-3 It should be suspected in patients with PJP who develop acute respiratory distress, even while on adequate medical treatment.2,4,5 It can evolve into a tension pneumomediastinum, which is a potential life-threatening complication.1,6
Figura I
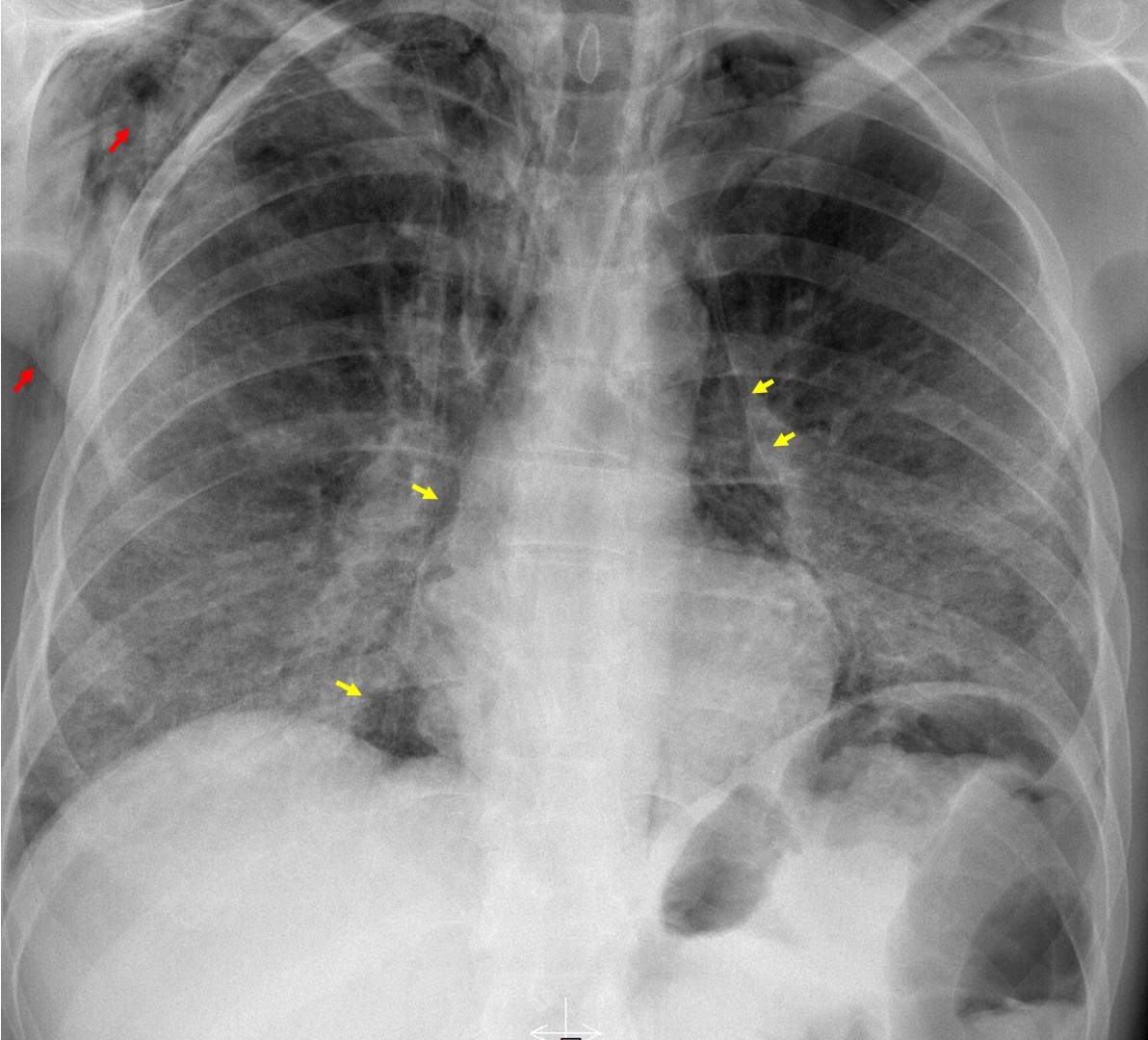
Chest radiograph showing an extensive pneumomediastinum (yellow arrows) and subcutaneous emphysema (red arrows).
Figura II
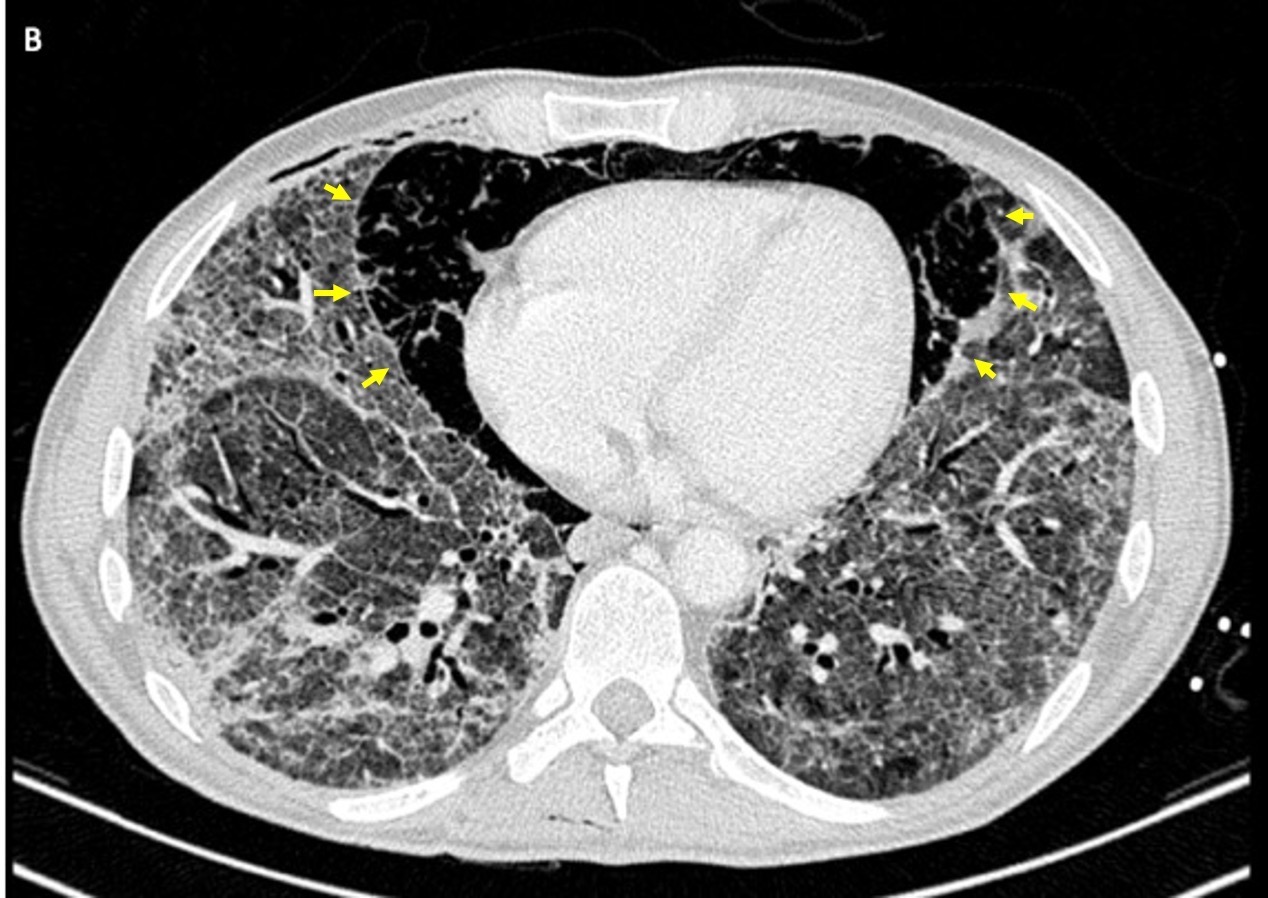
Chest computed tomography showing an extensive pneumomediastinum (yellow arrows) and diffuse bilateral ground glass opacities, interstitial thickening and small cysts (pneumatoceles).
BIBLIOGRAFIA
1. Cheng WL, Ko WC, Lee NY, Chang CM, Lee CC, Li MC, et al. Pneumomediastinum in patients with AIDS: a case report and literature review. Int J Infect Dis. 2014;22:31-34. Doi: 10.1016/j.ijid.2013.12.009.
2. França M. Pneumonia por Pneumocystis Jirovecii complicada por pneumotórax, pneumomediastino e enfisema subcutâneo. Acta Radiológica Portuguesa. 2016;28(107):25-26. Doi: 10.25748/arp.12001.
3. Saleem N, Parveen S, Odigwe C, Iroegbu N. Pneumomediastinum, pneumorrhachis, and subcutaneous emphysema in Pneumocystis jiroveci pneumonia in AIDS. Proc (Bayl Univ Med Cent). 2016;29(2):188-190. Doi: 10.1080/08998280.2016.11929412.
4. Yee D, Fu D, Hui C, Dharmadhikari N, Carino G. A Rare Case of 4 Ps: Bilateral Pneumothoraces and Pneumomediastinum in Pneumocystis Pneumonia. R I Med J (2013). 2020;103(5):52-54.
5. Cho JY, Kim DM, Kwon YE, Yoon SH, Lee SI. Newly formed cystic lesions for the development of pneumomediastinum in Pneumocystis jirovecii pneumonia. BMC Infect Dis. 2009;9(1):171. Doi: 10.1186/1471-2334-9-171.
6. Clancy DJ, Lane AS, Flynn PW, Seppelt IM. Tension pneumomediastinum: A literal form of chest tightness. J Intensive Care Soc. 2017;18(1):52-56. Doi: 10.1177/1751143716662665.