BACKGROUND
Male GCTs account for only 2% of all human malignancies. However, they are the most common cancer in young males (between 20 and 40 years old), with less than 2% of them being diagnosed over 55 years of age.1 Histologically, GCTs are divided into seminomatous (SE) and non-seminomatous tumors (NSE). SE GCTs retain the morphology of spermatogonial germ cells and are very sensitive to radio and chemotherapy, in contrast to NSE GCT, which display embryonal or extra-embryonal differentiation patterns, being much less sensitive to radiotherapy.2 Extragonadal GCTs are a rare subgroup of germ-cell neoplasms, most of them arising in the anterior mediastinum.3 Primary mediastinal GCTs (PMGCT) account for 15% of adult anterior mediastinal cancers and 1-3% of all germ cell malignancies can be associated with Klinefelter’s syndrome and hematologic malignancies.4 In the majority of cases (70-80%), PMGCT are NSE.1 Choriocarcinoma is an even more rare subgroup of PMGCT, especially in men, frequently accompanied by distant metastases.5 Choriocarcinoma, a highly malignant tumor from syncytiotrophoblast, can excrete β-hCG.5 The differential diagnosis of an anterior mediastinal mass is challenging, but high levels of β-hCG strongly suggest a PMGCT and a biopsy showing a mixed pattern between the cytotrophoblast and the syncytiotrophoblast reveals the presence of primary mediastinal choriocarcinoma (PMC) if no primary tumors are detected in the gonads.6
CASE PRESENTATION
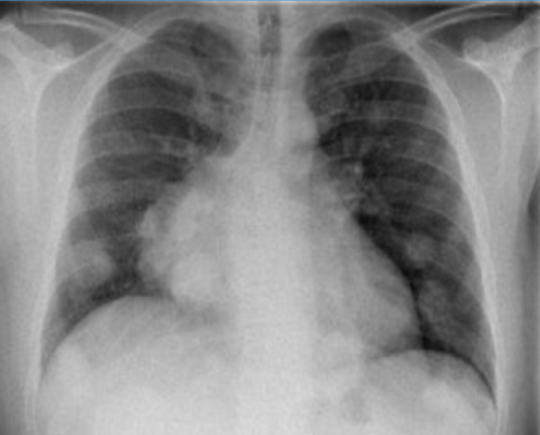
A 34-year-old man, without previous medical history, presented in the emergency service with a week lasting non-productive cough and hemoptysis on the day before. He also referred pleuritic pain and gynecomastia of the right breast, for a month. Physical examination showed a supra-nipple swelling in the right breast, in comparison with the left one, and body mass index of 27,3 kg/m.2 He was eupneic, without oxygen therapy, but with mild hypoxemia on arterial blood gases. No testicular masses were palpated and no other changes were detected on physical examination. Blood tests had lactate dehydrogenase elevation (2.8 ULN), with no other abnormalities. The chest x-ray showed bilateral pulmonary nodules and mediastinal widening (Fig. 1). The patient was admitted to the Internal Medicine ward to further workup.
Legionella, Mycoplasma, Cytomegalovirus, HIV 1 and 2 and viral hepatitis search was negative. Interferon-gamma release assay was positive, but no mycobacteria was found in biological fluids.
The high β-hCG value (12000 ULN) contrasted with other tumor markers, which were normal, including alpha-fetoprotein (AFP). Serum androgen levels were normal. However, follicle stimulating hormone (FSH) and luteinizing hormone (LH) levels were lower. Significant increases were found concerning estradiol (9 ULN), prolactin (3 ULN) and progesterone (8 ULN).
Testicular and abdominal ultrasound exams were performed, but with no tumor suspicion. Breast ultrasound showed signs of bilateral gynecomastia without other alterations.
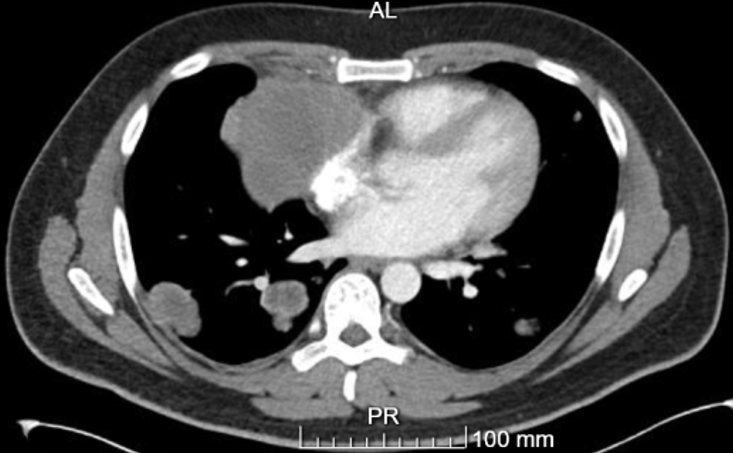
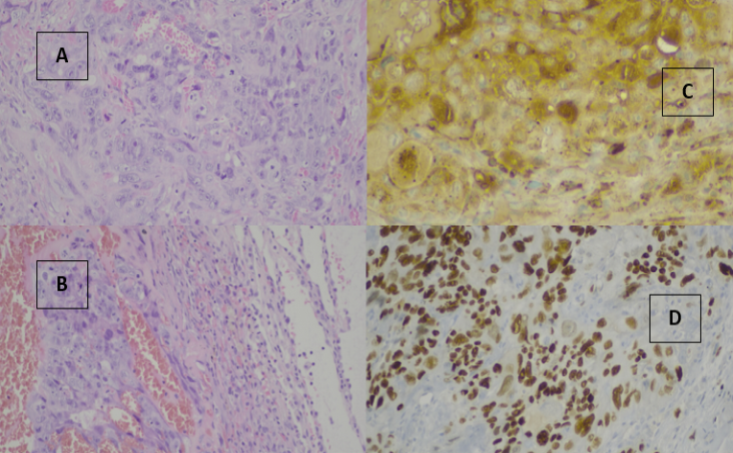
A thoracoabdominopelvic computed tomography (CT) showed a large mass located in the right anterior mediastinum, measuring 93x16x91 mm, extending from the pre-vascular space to the right cardiophrenic angle, presenting areas of liquefaction/necrosis inside. The mass was in contact with the anterior chest wall as well as with the ascending aorta and this mass deforms the superior vena cava and middle lobar vein (Fig. 2). CT also showed several dispersed bilateral pulmonary nodes, leading to suspicion of pulmonary metastasis. Once CT guided biopsy of mediastinal mass was inconclusive, the patient was submitted to thoracotomy and a pulmonary nodule was resected. The patient’s clinical condition deteriorated, accompanied by an increase in size and number of pulmonary nodules (Fig. 3). Considering the clinical condition and the strong suspicion of GCT, he started chemotherapy (QT) with bleomycin, etoposide and cisplatin after written informed consent, and sperm sample collection for cryopreservation, even before histopathological results. Before QT, treatment with isoniazid was initiated, assuming a potential latent tuberculosis. Pathology reported pulmonary metastasis of germinative cell tumor, large cells of syncytiotrophoblast and cytotrophoblast type, with strong and diffuse CK7, β-hCG and sall4 expression, indicating choriocarcinoma (Fig. 4). Given the fact that the testicular physical examination and the ultrasound had no alternation, choriocarcinoma of primary mediastinal origin was diagnosed. Therefore, the patient was transferred to the Urology department and after four cycles of QT (4 months) he was clinically stable, with a significant blood β-hCG value reduction (785 ULN)).
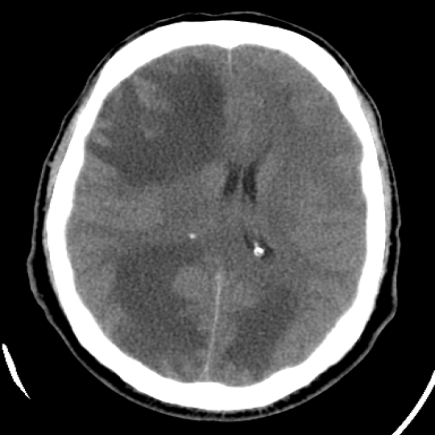
Three days after the last QT cycle, he was admitted in the emergency room, due to sudden severe headache associated with nausea and vomits. Head CT showed several brain metastases (Fig. 5). Corticotherapy was initiated (10 mg bolus of iv dexamethasone, followed by 5 mg, 2 times a day, per os) and holocraneal radiotherapy was performed. Despite QT, the disease progressed and the patient returned to the emergency room with similar symptoms, associated with seizure. He did not recover and died on the following day.
DISCUSSION
The diagnosis of a PMGCT should be considered in all young men with supraclavicular, retroperitoneal or mediastinal masses.7 In these patients, it is mandatory to perform a rigorous physical examination as well as blood levels of AFP and β-hCG determination.7
The diagnosis of PMC has to be taken into consideration when there is a report of choriocarcinoma and no primary tumors are detected in the gonads or in any location other than the mediastinum.8It is a very rare and aggressive tumor, associated with poor prognosis in short time6, with very unspecific and late symptoms.6 Chest pain, dyspnea and cough are usually the first symptoms to appear, related to mediastinum widening.1Cough, gynecomastia and chest pain constitute a very characteristic triad of PMC.8
Gynecomastia is related to the production of chorionic gonadotropin, which stimulates Leydig cells to produce testosterone and estrogen.8This estrogen production may be the determining factor in the mammary gland hypertrophy so often seen.8 Testicular cancers presenting with gynecomastia are reported to have a worse prognosis, which needs to be confirmed with further studies.9
β-hCG is important not only for the diagnosis, but also for follow up and prognosis.5,7 Serological elevated lactate dehydrogenase is not specific, but rather an important prognostic factor, and should be determined before treatment.7
Despite rare, there are several reported cases of this condition, as a recent one describing a 26-year-old patient with similar symptoms and diagnostic gait, as the patient we present, with a challenging pathology diagnosis.6 Several attempts might be needed, delaying the diagnosis, along with daily deterioration of the patient’s clinical condition. In some patients who are clinically unstable, with imminent risk of life and disease distribution consistent with the diagnosis of germ cell tumor, the beginning of QT may start even before histopathologic diagnosis and can be assumed in the presence of high serological β-hCG levels.10
Despite general high sensitivity of PMGCT to QT, there is no established protocol consistent with good results for PMC, especially if there is metastatic disease.8 The use of bleomycin, etoposide and cisplatin as first line therapy is usual in PMGCT even though the response is usually poor.7 Chemotherapy with etoposide, methotrexate, actinomycin D, cyclophosphamide and vincristine (EMA/CO) might be applied, and it was the regimen in some of the reported cases in literature, even though with reported rapid drug resistance and no significant outcome.6
In our case, there was a challenging early detection and diagnosis of PMC. It had been 1 month since the onset of initial symptoms until the first admission to the hospital. Because of the difficult diagnostic procedures, we had to carry out a new biopsy. Given the deterioration of the patient’s clinical condition he started QT with bleomycin, etoposide and cisplatin even before histopathological results. Despite initial improvement, the disease progressed even with QT.
In conclusion, PMC is one of most aggressive subtypes of GCT tumors, with very weak response to various QT regimens and with poor prognosis. The diagnosis is challenging, sometimes with histopathologic result not easily achieved, potentially delaying treatment initiation and worsening the patient’s prognosis.
Figura I
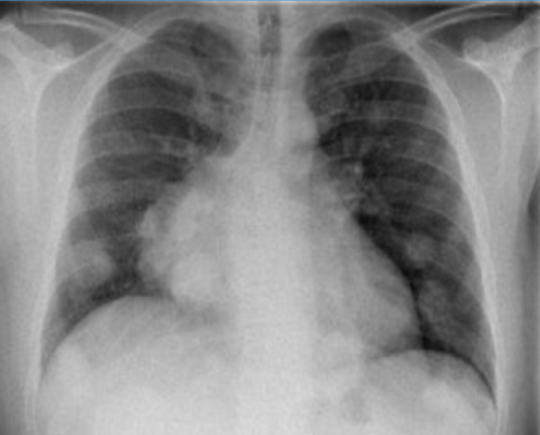
Initial chest x-ray with bilateral pulmonary nodules and mediastinal widening.
Figura II
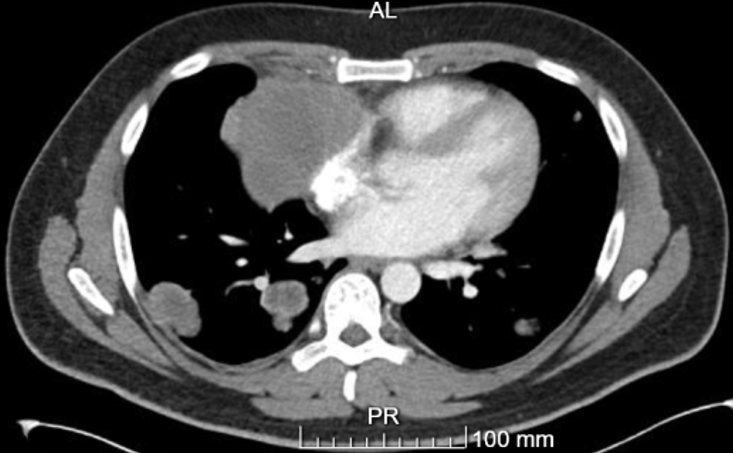
Large mass located in the right anterior mediastinum.
Figura III

Chest x-ray with increase in size and number of pulmonary nodules.
Figura IV
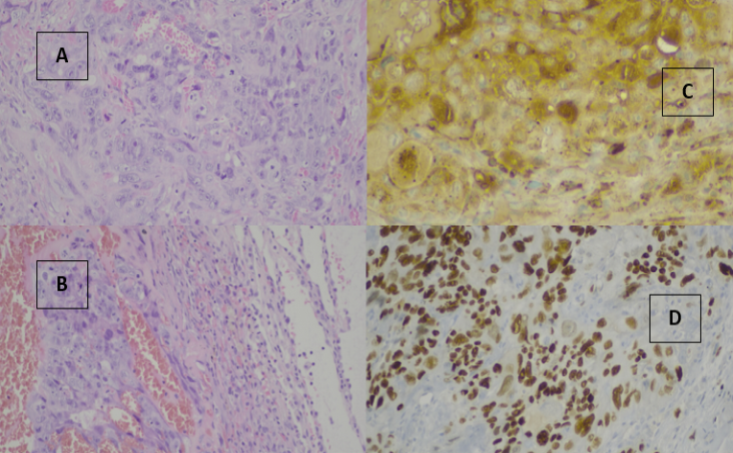
Pulmonary metastasis of choriocarcinoma. A and B HEX 200: large mass with anisocariosis and prominent nucleoli, in acinar and solid patterns. C and D: B-HCG and SALL4 expression in tumoural cells.
Figura V
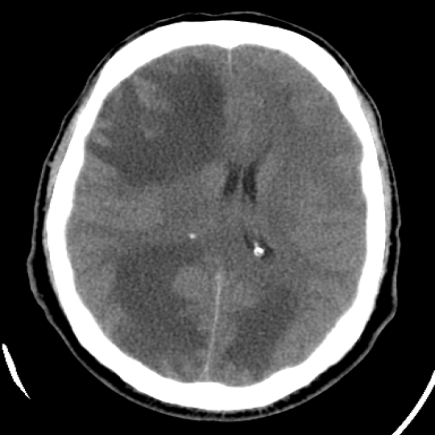
Brain metastasis of choriocarcinoma.
BIBLIOGRAFIA
1. Rosti G, Secondino S, Necchi A, Fornarini G, Pedrazzoli P. Primary mediastinal germ cell tumors. Semin Oncol. 2019 Apr;46(2):107-111. Doi: 10.1053/j.seminoncol.2019.04.001.
2. Houldsworth J. Genetics and biology of male germ cell tumors. Chest Surg Clin N Am. 2002;12(4):629-43. Doi: 10.1016/s1052-3359(02)00027-3.
3. Rodney AJ, et al. Survival outcomes for men with mediastinal germ-cell tumors: Yhe University of Texas M. D. Anderson Cancer Center experience. Urol Oncol. 2012; 30 (6): 879-85. Doi: 10.1016/j.urolonc.2010.08.005.
4. Kalhor N, Moran CA. Primary germ cell tumors of the mediastinum: a review. Mediastinum 2018;2:4. Doi: 10.21037/med.2017.12.01.
5. Zhang S, Gao H, Wang XA, et al. Primary choriocarcinoma in mediastinum with multiple lung metastases in a male patient: A case report and a review of the literature. Thorac Cancer. 2014;5(5):463-7. Doi: 10.1111/1759-7714.12120.
6. Qiu Z, Wu Y, Wang Y, Hu C. Male primary mediastinal choriocarcinoma with diffuse metastases: Medicine (Baltimore) 2019 Jul; 98(28): e16411. Published online 2019 Jul 12. Doi: 10.1097/MD.0000000000016411.
7. Honecker F et al. ESMO Consensus Conference on testicular germ cell cancer: diagnosis, treatment and follow-up. Ann Oncol. 2018 Aug 1;29(8):1658-1686. Doi: 10.1093/annonc/mdy217.
8. Gaude GS, Patil P, Malur PR, et al. Primary mediastinal choriocarcinoma. South Asian Journal of Cancer. 2013 Apr;2(2):79. Doi: 10.4103/2278-330x.110495.
9. Polat AV at al. Is gynecomastia related to the disease characteristics and prognosis in testicular germ cell tumor patients?. Diagn Interv Radiol. 2019;25(3):189-194. Doi:10.5152/dir.2019.18297.
10. Chan Wah Hak C, Coyle C, Kocache A, et al. Emergency Etoposide-Cisplatin (Em-EP) for patients with germ cell tumours (GCT) and trophoblastic neoplasia (TN). BMC Cancer. 2019;19(1):1-9. Doi: 10.1186/s12885-019-5968-7.