Introduction:
The primary cardiac lymphoma (PCL) is a rare form of both cardiac tumors and lymphomas, accounting for 0.5% of all lymphomas, and 1 to 3 % of the malignant cardiac tumors.1–3
By definition, PCL is a lymphoma that is localized inside the pericardial cavity. The severity of PCL depends on the localization of the tumor as it can grow in or into any cardiac or pericardiac tissue. Its clinical presentation includes arrythmias (from benign to fatal), rapidly progressive heart failure, pericardial effusion and systemic embolization.
Although extremely rare, PCL is more commonly seen in immunocompromised patients (such as Human Immunodeficiency Virus positive patients) but can also occur in immunocompetent patients. There is a male predominance and the median age at diagnosis is usually between 60 and 70 years old.4 Congestive heart failure and dyspnea are the most frequent presentations. Chest pain and B symptoms are frequent in later stages.3
The clinical manifestations depend on the disease’s location as it can invade any cardiac tissue (Endocardium/Myocardium/Epicardium/Pericardium) as well as cardiac cavities (atrii/ventriculi).5,6 Examples of these variable presentations include tumor growth into the right atrium leading to superior vena cava syndrome and/or pulmonary embolism, and left atrium or ventricular growth leading to systemic emboli. Cardiac arrythmias are also described in PCL patients,2 as these can range from benign to malignant which can lead to sudden death.7 Epicardium and pericardium involvement can result in massive pericardial effusion,5 which can lead to cardiac tamponade if left untreated. It is difficult to assess what is the most common presentation as there are few case series reported in the literature. Case reports in immunocompetent patients appear to demonstrate a frequent association of PCL with a cardiac mass.8
The diagnosis of PCL is made by histological and clinical criteria (all of the four should be met):
1) Tissue sampling via direct biopsy, open resection, or pericardial cytology;
2) Malignant lymphoid cells are centered in myocardium and/or Pericardium;
3) Clinical presentation reflects tumor’s impact on heart and/or Pericardium;
4) Extracardiac lymphoma is minimal to nonexistent in PCL.1
The prognosis of PCL is poor if left untreated,8 but there is usually an improvement if chemotherapy is performed.8 However, it still has a median overall survival of 12 months after diagnosis.1 The most wildly used therapeutic regimen is R-CHOP: rituximab (R) (increases overall survival and remission rates), cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) therapy. One review article reported complete response rate of 59% and overall response rate to chemotherapy of 79%.4Cardiac surgery is reserved to life-threatening conditions and as it does not improve survival rate.4
We present the case of an 80-year-old woman who was referred by her family doctor to the emergency department with rapidly progressive heart failure due to a large pericardial effusion secondary to PCL. This is a relevant case report as PCL is an extremely rare cause of heart failure with pericardiac effusion and has a high mortality rate if left undiagnosed and untreated.
Case description
We present a case of an 80-year-old woman, who had history of essential hypertension, dyslipidemia, type 1 obesity and was chronically medicated with pantoprazole 20mg, acetylsalicylic acid 100mg, lisinopril 5mg, hydrochlorothiazide 12.5mg and simvastatin 40mg.
She presented at the emergency department with progressive heart failure starting two weeks prior to admission, characterized by breathlessness, palpitations, paroxysmal nocturnal dyspnea, dyspnea at rest, weight gain, orthopnea, oedema of lower limbs. She denied fever (above 38ºC), sweating and weight loss. She denied any previous heart disease.
On her physical examination she was tachycardic, but rhythmic with muffled heart sounds and fine pulmonary crackles on auscultation. She also presented with signs of fluid overload such as peripheral oedema and hepatojugular reflux. No adenomegaly were found.
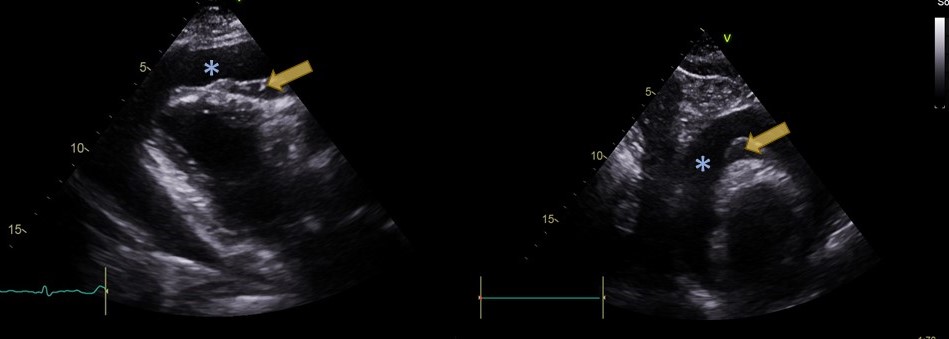
The blood analysis showed dilutional anemia and normal LDH (unlike effusions’ LDH) (Table 1 and 2). Sinus tachycardia (130 beats per minute) and low voltage QRS complexes were found on her electrocardiogram. She also performed a 24-hour HOLTER exam which revealed paroxysmal atrial fibrillation. Transthoracic echocardiogram revealed “large pericardial effusion (anterior axis 29mm, posterior 23mm) with deposits of fibrin/secondary deposits” (Figure 1). Diagnostic and therapeutic pericardiocentesis was performed, and its analysis was compatible with an exudate as it showed increased LDH (Table 2). Cytology analysis had “Pericardial fluid with abundance of atypic lymphocytes, with large and polymorph nuclei. Immunohistochemical analysis was positive for CD20 and negative for CD3 and CD5, compatible with non-hodgkin B cell lymphoma”.
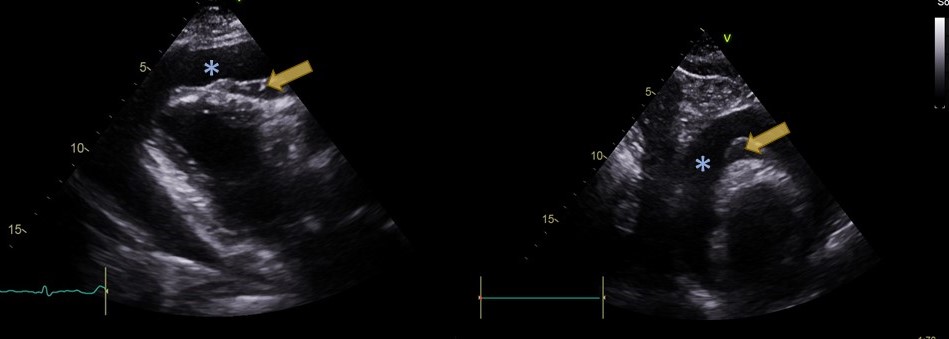
Bone marrow biopsy showed no medullary involvement and the body Positive Emission Tomography reported only pathological findings in the pericardium (PET-CT): Perithoracic-aorta, Infundibulum and Apex (Figure 2), thus extracardiac disease was excluded.
After the final diagnosis was established the patient’s, clinical case was submitted to a multidisciplinary meeting. The possibility of performing a tissue biopsy (myocardium/pericardium) was discussed but was dismissed as it would not interfere with the therapeutic plan or and would have unnecessary risks. Thus, the diagnosis of Primary Cardiac B Cell non-Hodgkin lymphoma was made and the patient started on chemotherapy. R-CHOP was started (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone) and remission was achieved after the first chemotherapy cycle. The patient has been in remission for 5 years with maintenance therapy (rituximab) with no recurrence of pericardiac effusion, other cardiac signs or symptoms or PET-CT lymphoma associated lesions.
Discussion
In this particular case, the patient presented with symptoms of progressive heart failure due to pericardial effusion. The transthoracic echocardiogram findings and the highly increased LDH in the pericardiac liquid made us consider primary or secondary malignancy.
The diagnostic criteria of PCL were met: the patient’s pericardial cytology obtained by pericardiocentesis showed non-hodgkin B cell lymphoma cells; malignant lymphoid cells were restricted to the epicardium and pericardium and this resulted in presentation with heart failure secondary to pericardial effusion and epicardial mass. PET-CT showed no extracardiac locations of the disease.
Some factors greatly benefited this patients’ prognosis:1 R-CHOP therapy was promptly initiated; the disease was localized in the epicardium/pericardium and the pericardial effusion resolved with the therapy, so no cardiac surgery was needed; there were no severe complications of the disease at the time of presentation such as life-threatening arrhythmias, cardiac tamponade or pulmonary/systemic emboli.
Even though PCL is extremely rare, this diagnosis should be taken into account in cases of acute/sub-acute pericardial effusions (present in up to 50% of all PCL cases),8progressive heart failure and unexplained arrhythmias or cardioembolic events. Early diagnosis can be made using imaging techniques and cytology/biopsy an it is crucial as chemotherapy can induce clinical remission.
PCL is a challenging diagnosis as it has a very variable presentation and a rapid progression, therefore clinicians should be aware of this condition, as an early suspicion is key to a rapid and correct diagnosis.
Quadro I
Relevant Laboratory findings of Blood analysis
| | |
| Parameter | Value |
| Hemoglobin | 11.3g/dL |
| Leucocytes | 6500 10^6/L with regular distribution |
| Creatinine | 0.7mg/dL |
| Lactate dehydrogenase (LDH) | 270 U/L (normal) |
| Total Protein | 6.9g/dL |
| NT-proBNP | 105pg/mL |
| HIV (1 and 2) Antibodies | Not Present |
NT-proBNP: NT-proB-type Natriuretic Peptide
Quadro II
Relevant Laboratory findings of pericardiac liquid analysis
| | |
| Parameter | Value |
| Lactate dehydrogenase | 81660 U/L (increased) |
| Glucose | 29 mg/dL |
| Total Protein | 6 mg/dL |
Figura I
Echocardiogram: (*) Pleural Effusion; (arrow) Epicardic/Pericardic deposits
Figura II

Pre-Treatment PET-SCAN - (arrow) Peri-aorta (SUVmáx. 6,3); (*) Infundíbulum (SUVmáx. 4,1); (+) Apex (SUVmáx. 3,9);
BIBLIOGRAFIA
1. Jeudy J, Burke AP, Frazier AA. Cardiac Lymphoma. Radiol Clin North Am. 2016 Jul;54(4):689–710.
2. Jonavicius K, Salcius K, Meskauskas R, Valeviciene N, Tarutis V, Sirvydis V. Primary cardiac lymphoma: two cases and a review of literature. J Cardiothorac Surg. 2015 Dec;10(1):138.
3. Lamba G, Frishman WH. Cardiac and Pericardial Tumors: Cardiol Rev. 2012;20(5):237–52.
4. Chen H, Qian S, Shi P, Liu L, Yang F. A presentation, treatment, and survival analysis of primary cardiac lymphoma cases reported from 2009 to 2019. Int J Hematol. 2020 Jul;112(1):65–73.
5. Petrich A, Cho SI, Billett H. Primary cardiac lymphoma: An analysis of presentation, treatment, and outcome patterns. Cancer. 2011 Feb 1;117(3):581–9.
6. Patel J, Melly L, Sheppard MN. Primary cardiac lymphoma: B- and T-cell cases at a specialist UK centre. Ann Oncol. 2010 May;21(5):1041–5.
7. Cheng J-F, Lee S-H, Hsu R-B, Yu S-C, Shun C-T, Huang P-S, et al. Fulminant primary cardiac lymphoma with sudden cardiac death: A case report and brief review. J Formos Med Assoc. 2018 Oct;117(10):939–43.
8. Miguel CE, Bestetti RB. Primary cardiac lymphoma. Int J Cardiol. 2011 Jun;149(3):358–63.