We report the case of a 56-year-old white female admitted to the emergency department due to hypoglycaemic coma. After reversion of unconsciousness, she remained with asymptomatic low glycaemic levels, despite oral feeding and continuous i.v. 10% glucose infusion. She reported a 10 pack-year tobacco history, depression and sideropaenic anaemia. She complained of fatigue walking uphill, for the past three months and digital clubbing, for the past two years. Physical examination presented a thin female, heart rate was 111 beats/min, tympanic temperature was 38,7ºC and peripheral oxygen saturation was 90%. Percussion of the left hemithorax was dull, with absent tactile fremitus and ipsilateral abolished breath sounds on pulmonary auscultation. Her fingers were long with digital clubbing. The remainder of the physical examination was unremarkable. Her laboratory results were normal (including Haemoglobin, Leukocyte, platelet count, creatinine, ionogram, urea, free-T4 and TSH), apart from low levels of glycaemia, Insulin and C-peptide, high erythrocyte sedimentation rate (80 mm/h) and her IGF-2 was normal. A chest radiograph showed a diffuse left hemithoracic opacity (Fig. 1). A Thoracic CT was performed, obtained with the administration of contrast media, revealed complete left lung collapse, conditioned by the presence of left pleural effusion and large, confluent, heterogeneous masses that filled the entire left pleural cavity, pushing the mediastinum to the right and the left hemidiaphragm caudally, without invasion of adjacent structures (Fig. 2). A transthoracic CT-guided biopsy was performed and tissue histology revealed mesenchymal fusocellular neoplasm (Vimentine+; CD34+; BCL2+; CD99+; Ki67-10%), with increased mitosis, in favour of malignant solitary fibrous tumour of the pleura (SFTP). She underwent en-bloc excision of the tumour, via left thoracotomy. The mass was a giant polilobulated tumour, with cystic and solid areas, highly vascularized and with adhesions to the anterior chest wall and to the lung, with positive surgical margins. On the 6th month after surgery, there was evidence of tumour relapse. She underwent exploratory thoracotomy and, because of intraoperatively established non-resectability, biopsy samples were taken, confirming tumour progression. Due to worsening clinical condition, she was admitted to inpatients for palliative care, dying 10 months after the initial diagnosis.
SFTP is a tumour of mesenchymal origin, whose course can be benign or malignant.1 Rarely SFTP presents with paraneoplastic syndromes as Doege-Potter syndrome (DPS). DPS as first described by Doege2 presents as a fibrous tumour with symptomatic hypoglycaemia that may either ectopically excrete IGF-2 or is related to increased tumour size, malignant tumours or with high mitotic rate.3 This is rare case of a SFTP with DPS.
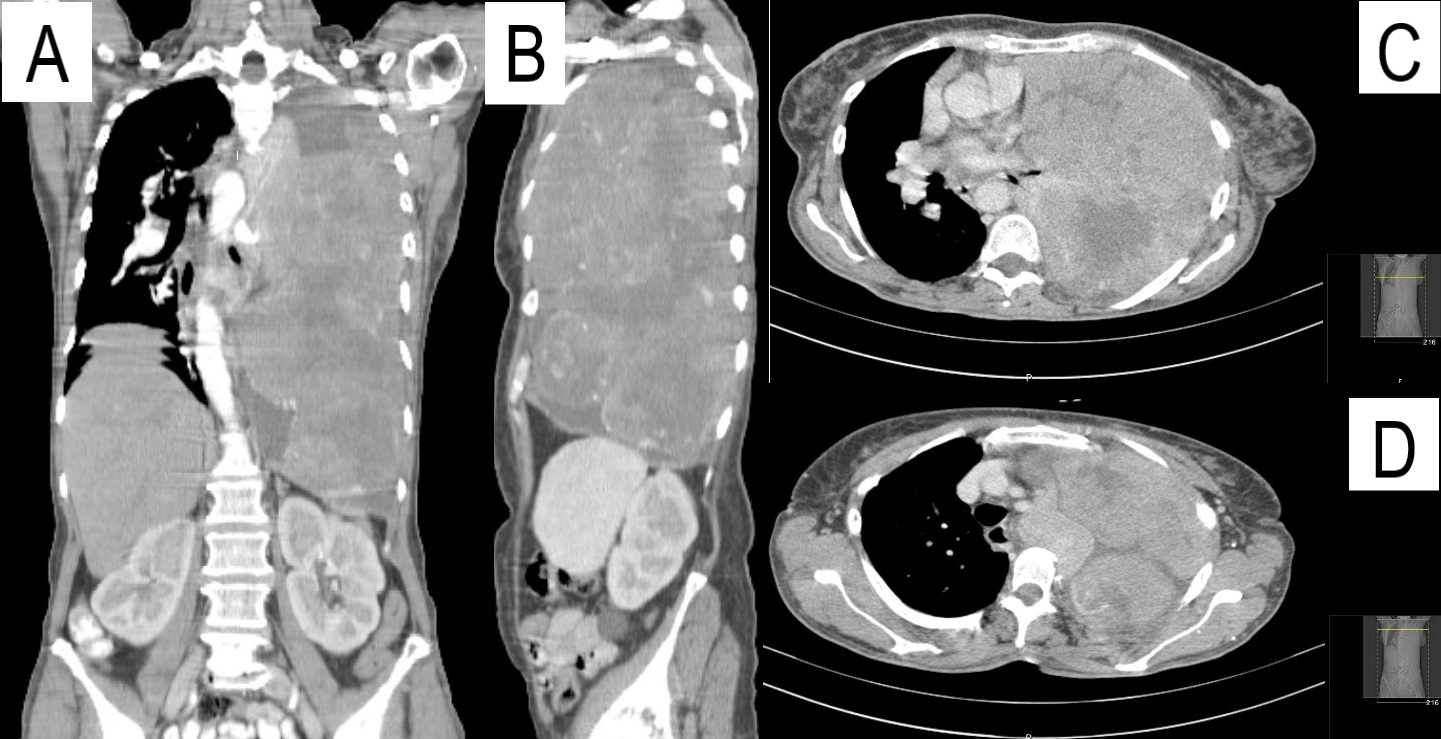
Figura I

Chest posteroanterior roentgenogram.
Figura II
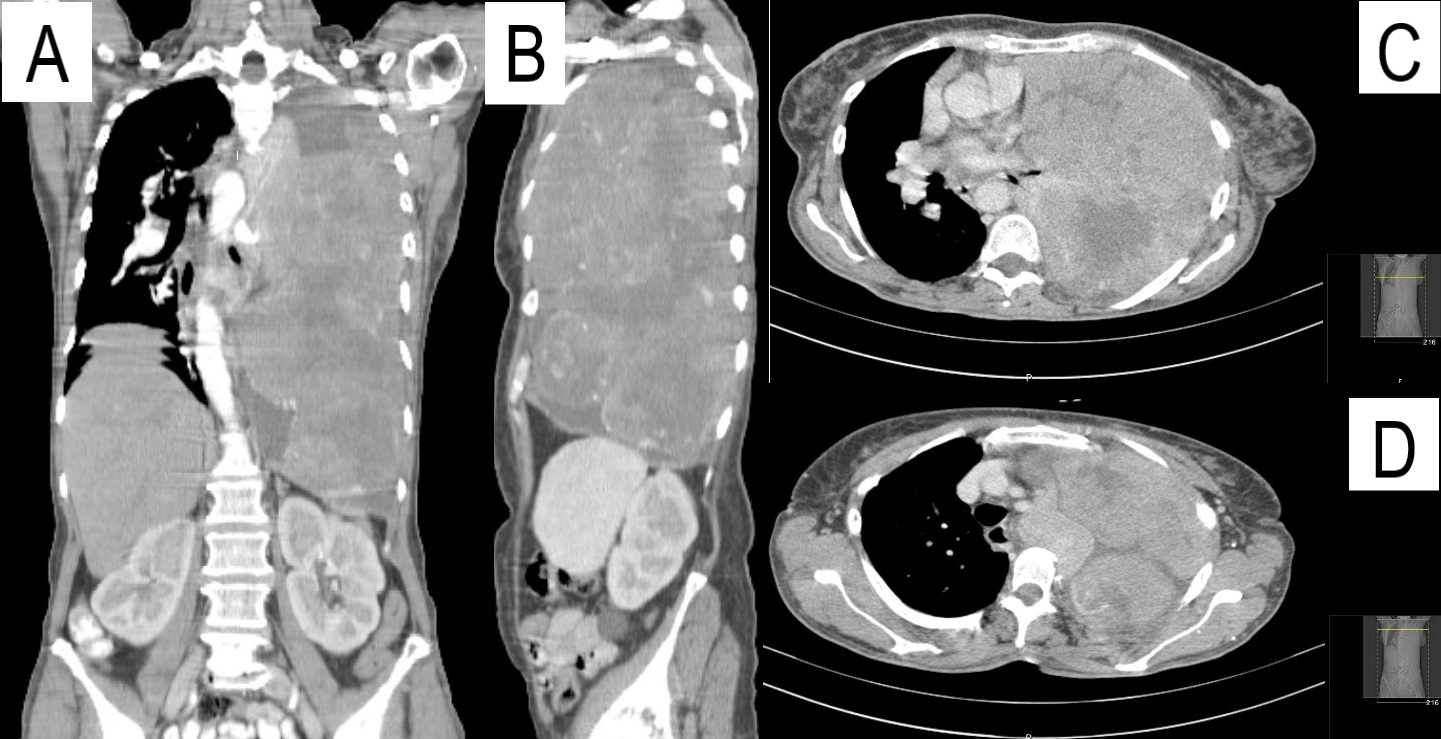
CT scan after intravenous contrast. Multiple heterogenous masses filling the entire left pleural cavity. (Panel A Coronal view; Panel B Sagital view; Panel C and D Axial view)
BIBLIOGRAFIA
(1) Rena O, Filosso PL, Papalia E, Molinatti M, Di Marzio P, Maggi G, Oliaro A: Solitary fibrous tumour of the pleura: surgical treatment. Eur J Cardiothorac Surg. 2001, 19:185-189
(2) Doege KW. FIBRO-SARCOMA OF THE MEDIASTINUM. Ann Surg. 1930;92(5):955-960.
(3) Han G, Zhang Z, Shen X, Wang K, Zhao Y, He J, Gao Y, Shan X, Xin G, Li C, Liu X. Doege-Potter syndrome: A review of the literature including a new case report. Medicine (Baltimore). 2017 Jul;96(27):e7417