Swyer-James-MacLeod’s Syndrome (SJM), also known as unilateral hyperlucent lung syndrome, is an uncommon disease that results in decreased pulmonary vascularity and hyperinflation that may be confined to one lung or one lobe, with or without bronchiectasis.1,2
The condition was first described simultaneously in the 1950s by a respiratory physician William Mathieson Macleod in England (1954) and by a physician Paul Robert Swyer and a radiologist George James in Canada (1953).2
One study reported a prevalence of 0.01% in a series of 17,450 reviewed chest radiographs.3
It was initially thought to be a congenital anomaly but is now recognized as a postinfectious form of bronchiolitis obliterans that can be caused by a variety of infectious agents, including adenovirus and measles.4
Many cases remain undiagnosed or are treated as other conditions, such as asthma or bronchiectasis due to the diagnostic challenges.
When symptomatic, patients most often present with recurrent pulmonary infections or exertional dyspnea. Other symptoms include wheezes, dyspnea on exertion, reduced exercise tolerance, cough (often productive) with or without hemoptysis, and pleuritic chest pain. Most patients, however, are asymptomatic.5
Therapy is aimed primarily at control of the intercurrent episodes of bacterial pneumonia. Surgery is rarely indicated.6
We describe an 19 -year-old patient, rugby player, with a history of asthma since 5 years old. The patient presented with cough and dyspnea on effort. Chest radiograph showed heterogeneous opacity of the right lung. Computed tomography revealed hyperlucent right lung with markedly reduced vascularity. Pulmonary function tests showed a forced expiratory volume in 1 second of 4.280 L (102% of expected value) and a forced vital capacity of 5.430 L (110% of expected value).
This report presents the computed tomographic (CT) appearance of this entity and also emphasizes the significant role CT may have in its diagnosis.
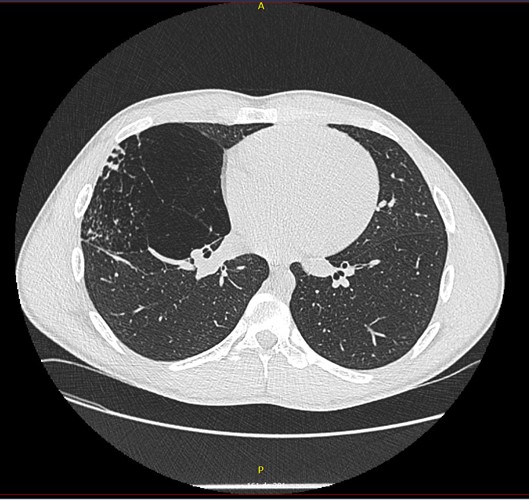
Figura I
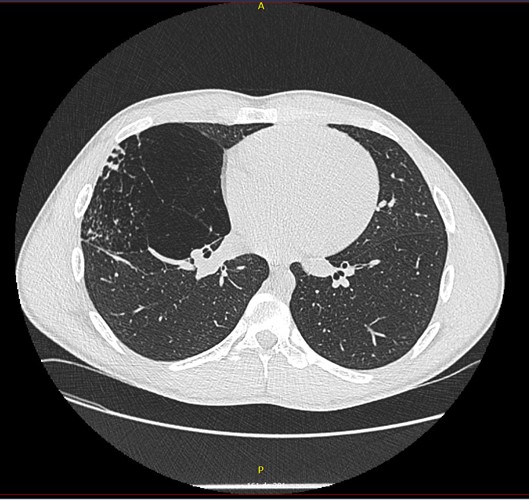
Chest high resolution computed tomography scan demonstrating hyperinflation (air trapping) in the pulmonary parenchyma
BIBLIOGRAFIA
1.Fregonese L, Girosi D, Battistini E, et al. Clinical, physiologic, and roentgenographic changes after pneumonectomy in a boy with Macleod/Swyer-James syndrome and bronchiectasis. Pediatr Pulmonol 2002; 34:412.
2.Daniel TL, Woodring JH, Vandiviere HM, Wilson HD. Swyer-James syndrome--unilateral hyperlucent lung syndrome. A case report and review. Clin Pediatr (Phila) 1984; 23:393.
3.Sen HS, Taylan M, Abakay O, Sezgi C, Cetincakmak MG. Adult diagnosis of Swyer-James-Macleod syndrome: retrospective analysis of four cases. Respir Care. 2014 Apr;59(4):e51-4.
4.Capela, C., Gouveia, P., Sousa, M. et al.Adult diagnosis of Swyer-James-MacLeod syndrome: a case report. J Med Case Reports; 2011; 5, 2 ().
5.Dirweesh A, Alvarez C, Khan M, Shah N. A unilateral hyperlucent lung - Swyer-James syndrome: A case report and literature review.Respir Med Case Rep.2017;20:104-106.
6.Silva PS, Lopes R, Neto HM. Swyer-James-MacLeod syndrome in a surgically treated child: a case report and brief literature review. J Pediatr Surg 2012; 47:e17.