Introduction:
Capecitabine is a cytostatic agent widely used in the treatment of many neoplasms, namely of digestive tract and breast. However being efficient it may carry adverse effects as many other useful drugs. Unstable angina and myocardial infarction were reported as infrequent (incidence of 1/1000 to 1/100) and arrhythmia or coronary vasospasm as rare (incidence of 1/10000 to 1/1000) adverse effects. In literature there are some reports of cardiac adverse effects induced by capecitabine. With this case report we intent to alert the healthcare professionals about rare presentations of a drug adverse event.
Narrative:
We present the case of a 49-year-old man, which attended the emergency department (ER) with excruciating oppressive chest pain, irradiating to his left upper limb and chin, with associated hypersudoresis and cutaneous pallor. The symptoms had started 30 minutes before, with no identified precipitant factors. He stressed that the day before he had had a similar episode, lasting 20 minutes, with spontaneous resolution.
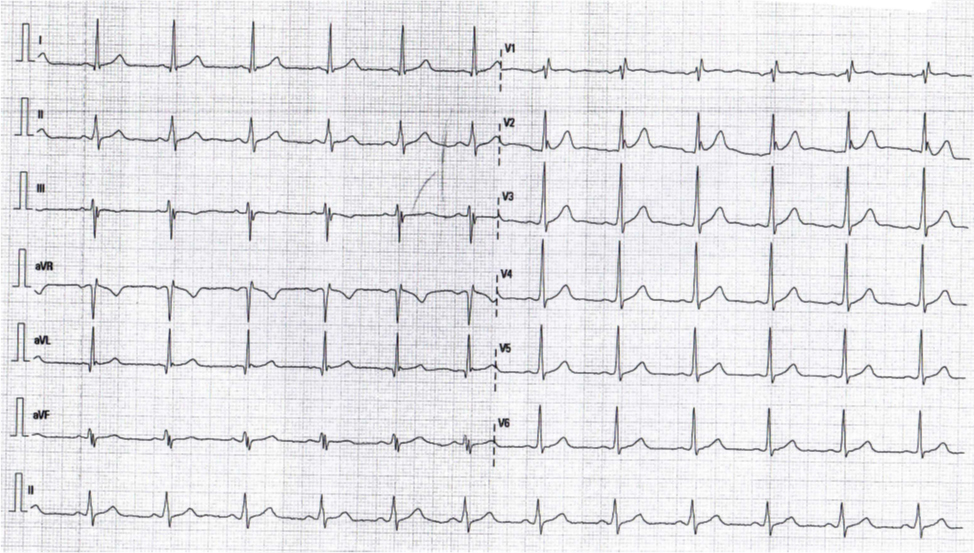
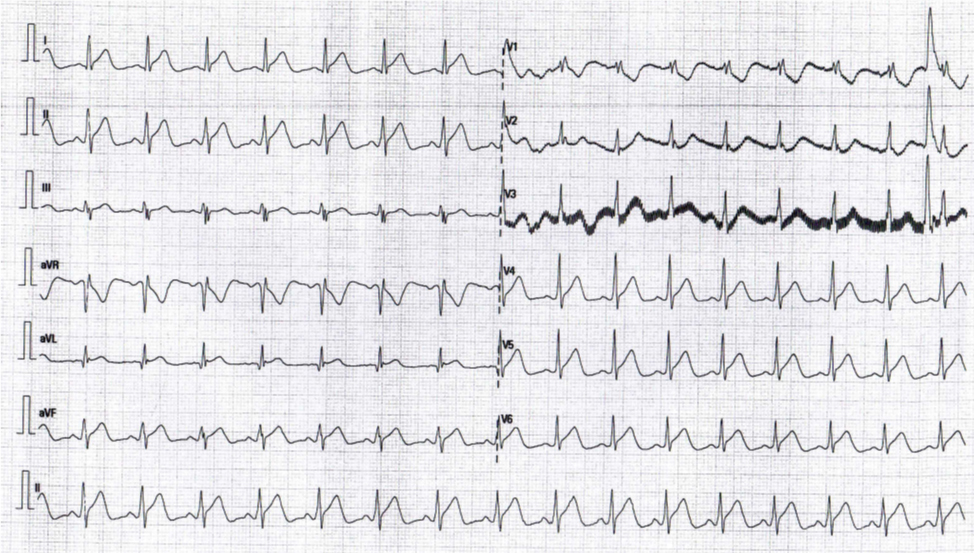
He had a recent diagnosis of rectal adenocarcinoma, submitted to chemotherapy and neo-adjuvant radiotherapy. No other relevant past medical history was reported, besides hypo-chromic microcytic anemia. Three days before he started capecitabine per-os, in monotherapy, and no other current medications were reported. There was no relevant family or psychosocial history, and none genetic disorders. Physical examination was normal including vital signs. Meanwhile the pain had resolved spontaneously (globally lasting less than 35 minutes). Initial 12-lead EKG (Fig. 1) revealed sinus rhythm and a right branch block pattern. Chest X-ray was normal and baseline cardiac troponin I was bellow reference values. During ER stay, the patient developed thoracic pain, similar to the previous episode, after minor effort. EKG performed during pain (Fig. 2) revealed generalized upper elevation of the ST-segment, which normalized after administration of sublingual dinitrate and resolution of the chest pain. Serial dosing of serum cardiac troponin I has remained below reference values. He underwent left cardiac catheterization with coronarography which revealed no coronary artery disease (Fig. 3). Hence, the diagnosis of coronary vasospasm induced by capecitabine was considered.
The patient was admitted for 48h and treated with transdermic nitrate and a calcium channel blocker. Capecitabine was discontinued and no more thoracic pain or EKG alterations were reported, even after discharge. Currently, the patient has no cardiac targeted therapy and is doing well for this point of view. In what concerns colorectal cancer, he has undergone alternative chemotherapy regimens.
Discussion:
Capecitabine is an oral prodrug that is converted to its only active metabolite, 5-fluorouracil (5-FU), and was developed with the goal of improving tolerability and intra-tumor drug concentrations through tumor-specific conversion to the active drug. Capecitabine has shown varying degrees of efficacy with acceptable tolerability in numerous neoplasms, namely in metastatic breast and colorectal cancers. However, it is not devoid of serious side effects, and even being less reported than 5-FU toxicity, capecitabine cardiotoxicity has already been pointed out in literature.1, 2 The mechanism of action is not clearly understood but may be endothelial-mediated, with a direct vasoconstrictor effect.3
Coronary vasospasm has been reported has a rare adverse effect of capecitabine,4,5 and in an emergency scenario we always have to rule out myocardial infarction, because of its lethal potential. Yet, performing a coronarography and finding no coronary disease supports the diagnosis, in this context. Treatment includes vasodilatation and discontinuation of capecitabine.
Rechallenging should be avoided because it carries a high risk of recurrence of the cardiac symptoms and prophylactic treatment is not always protective, so other chemotherapy alternatives should be pursued.6
Conclusions:
The main take-home message with this case report is that when considering potential life-threatening diagnosis in emergency scenarios we always have to remember about rare drug adverse effects.
Acknowledgements:
The authors acknowledge all the healthcare professionals who directly dealed with this patient, as well as the patient himself.
Figura I
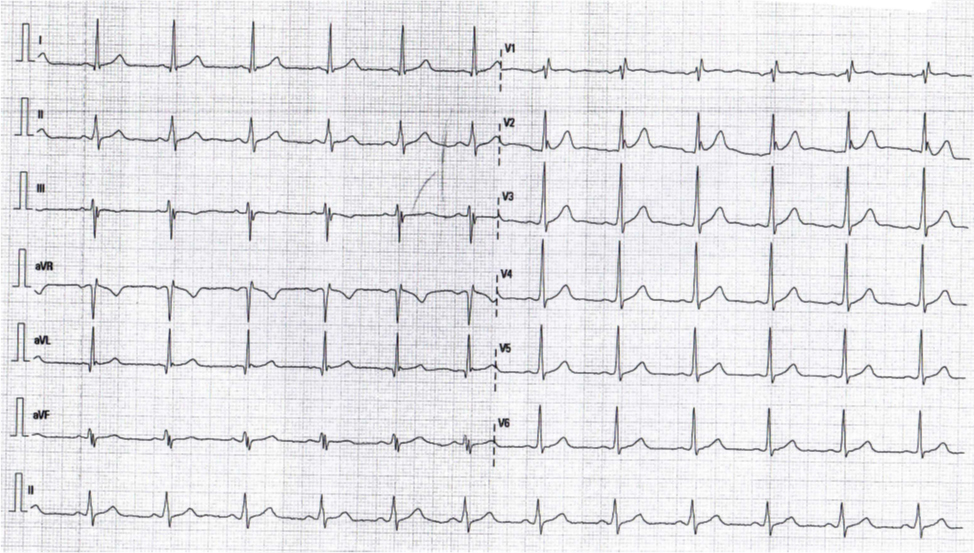
Admission EKG with sinus rhythm and a right branch block pattern
Figura II
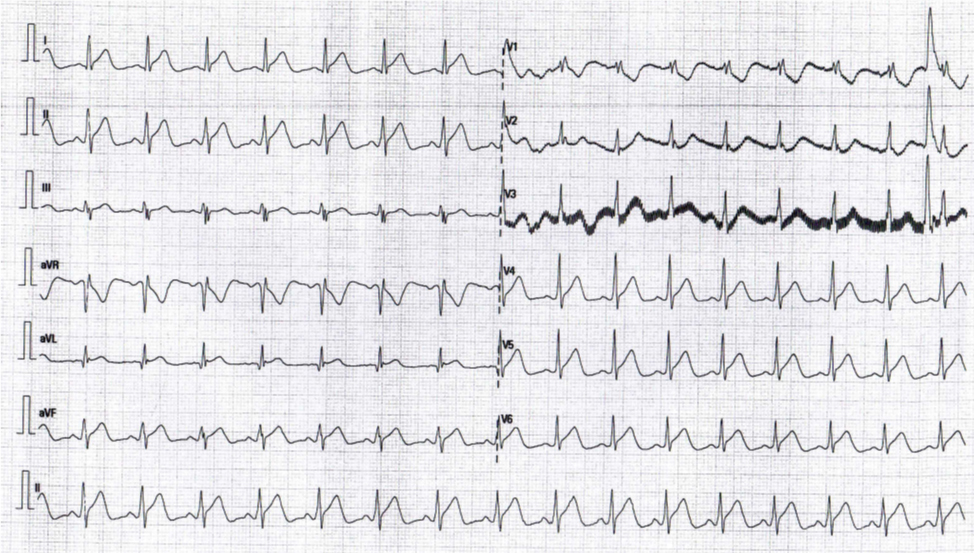
EKG during thoracic pain regarding generalized upper elevation of the ST-segment
Figura III

Coronarography revealing no coronary disease
BIBLIOGRAFIA
1. Anne Polk, Merete Vaage-Nilsen et al. Cardiotoxicity in cancer patients treated with 5-fluorouracil or capecitabine: a systematic review of incidence, manifestations and predisposing facts. Cancer Treatment Reviews 39 (2013): 974-984.
2. Mutahar Ali Tunio, Altaf Hashmi, Muhammad Shoaib. Capecitabine induced cardiotoxicity: a case report and review of literature. Pak J Pharm Sci, 2012 Jan; 25 (1): 277-81.
3. Morris Mosseri, Howard J Fingert, Lyuba Varticovski, et al. In vitro evidence that myocardial ischemia resulting from 5-fluorouracil chemotherapy is due to protein kinase C-mediated vasoconstriction of vascular smooth muscle. Cancer Research, 1993 jul 1 (53): 30M-3H33.
4. Danish Henry, Francine Rudzik, Allison Butts, Aju Mathew. Capecitabine-induced coronary vasospasm. Case Rep Oncol 2016; 9: 629-632; Doi: 10.1159/0450544.
5. Alfonso Sestito, Gregory Angelo Sgueglia et al. Coronary artery spasm induced by capecitabine. Journal of cardiovascular Medicine 2006, 7: 136-138.
6. Guido Deboever, Nick Hiltrop, Mike Cool, Guy Lambrecht. Alternative treatment options in colorectal cancer patients with 5-fluorouracil-or-capecitabine-induced cardiotoxicity. Clin Colorectal Cancer, 2013 Mar; 12 (1): 8-14. Doi: 10.1016/j.clcc.2012.09.003.