BackgroundDercum disease, also known as “Adiposis dolorosa” was first described in 1892 by Dr. Francis Xavier Dercum1-3 and it is characterized by the appearance of multiple painful subcutaneous lipomas.2,4 The most common areas of painful adipose tissue include the proximal extremities, trunk and buttocks. Pain is classically described as aching, stabbing, or burning and it is generally symmetric. It typically worsens with palpation.3-5
Adiposis dolorosa mainly affects women aged 35–50 years old,2,4,6,7 with the ratio of women to men estimated at 5–30: 1.4,6 Although the original author’s proposal described a predominance of incidence in postmenopausal women, recent studies revealed that most patients develop the disease before menopause.2,4,7
Diagnosis is primarily clinical and other chronic pain syndromes should be excluded.5 In 2012, Hanson and his colleagues defined two cardinal manifestations that characterize this entity: generalized overweight or obesity and chronic pain (>3 months) in the adipose tissue.3,4 Other clinical features which have been historically considered diagnostic criteria of Dercum disease, such as asthenia and psychiatric disturbances, are now described as associated symptoms.4 In fact, on a survey with 110 patients, developed by Herbst and Asare-Bediako in 2007, 66.4% of people referred depression; 92.7% had sleep disturbances; 86% mentioned impaired memory and 66.4% had concentration difficulty.7
Adiposis Dolorosa’s aetiology is still unknown. Current hypotheses include nervous system dysfunction, endocrine disorder, lymphovascular and adipose tissue dysfunction, and trauma-induced injury. Most cases are found to be sporadic, but some studies also suggest an autosomal dominant pattern with variable penetrance.4-6
Management of Dercum disease has been largely unsatisfactory since available treatments are essentially symptomatic. Analgesics, non-steroidal anti-inflammatory drugs and opioids have usually a poor response.2,5,6 The use of intralesional lidocaine seems to block the neural conduction and alleviate pain for a short period of time.2,6 Other treatment modalities with mixed results of potential benefit include ketamine, methotrexate, infliximab, interferon alpha-2b, corticosteroids, calcium-channel modulators, intravenous deoxycholic acid, transcutaneous electrical stimulation, and rapid cycling hypobaric pressure.2,3,5,8-10 Liposuction and lipectomy may be effective for pain reduction, but still have a high risk of recurrence.2,3,5,8
We report a clinical case about a woman with Dercum disease which illustrates the importance of thinking about rare diagnosis after excluding the most frequent ones. Similarly to other cases of Adiposis dolorosa, a multidisciplinary approach, with the collaboration of Internal Medicine, Dermatology, Surgery, Pain specialists and Nutrition, revealed to be essential on therapeutic management of the disease.
Case ReportWe present a case of a 53-year-old female, with history of hypertension and obesity. Family history was irrelevant.
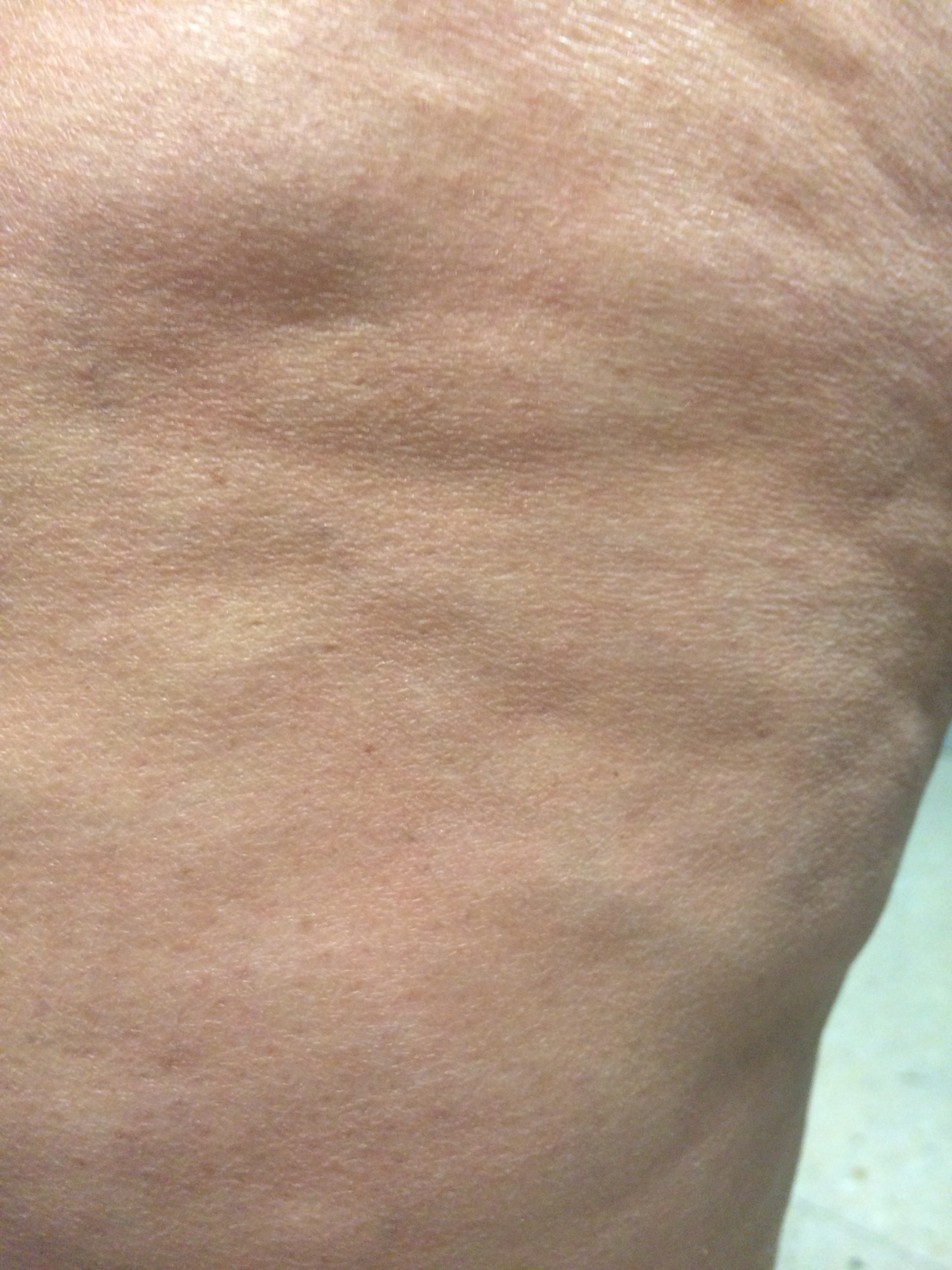
For 4 years, the patient had noticed multiple painful nodules with regular edges and elastic consistency, growing mainly in the abdomen and limbs (Fig´s 1-3). One year previously, she had also described similar lesions in her scalp, associated to itching and local ulceration (Figure 4). These nodular lesions were linked with a very intense paroxysmal pain, described as burning. Patient also mentioned asthenia, irritability, depressive mood, and emotional lability.
In the physical examination, the patient weighed 95 kg, corresponding to a body mass index of 40.6 kg/m2, and blood pressure was 174/89 mmHg. Several painful nodules were noticed across the abdomen and limbs. The biggest of them, located in the dorsal region, measured about 8 cm of longer axis. Many ulcerative lumps were objectified also on the scalp (Fig´s 1-4). Tender point test for fibromyalgia was negative. Remaining examination was irrelevant.
Laboratory tests were unremarkable, highlighting only a discreet change in lipids metabolism: total cholesterol of 208 mg/dL and HDL cholesterol of 49 mg/dL. Erythrocyte sedimentation rate, thyroid function, cortisol and remaining hormonal tests were normal. Autoimmunity study was negative.
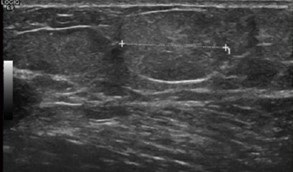
The patient underwent imaging exams, in order to characterize nodular lesions. The abdominal-pelvic CT documented: “Some areas of subcutaneous tissue focal thickening are found in anterior abdominal wall, which don’t consist in definitive lumps (wall lipomatosis?).” The soft tissue ultrasound of right elbow showed “hyperechogenic lumps, with 18 and 15 mm, compatible with lipomas” (Fig. 5).
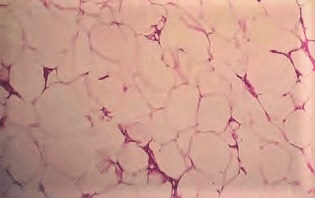
This case was discussed with Dermatology and General Surgery specialists and, considering the apparent benign nature of lesions, an excisional lump biopsy was performed. Anatomopathological exam of left forearm lump biopsy suggested “benign neoplasm constituted by mature fatty tissue, with several lines of fibrous tissue, which characterizes a lipoma.” (Fig. 6).
Differential diagnosis included Cushing syndrome, hypothyroidism, Fibromyalgia, panniculitis, Madelung syndrome and familial lipomatosis disorders. Considering that all laboratory study was negative, the anatomopathological exam was consistent with lipomas and family history was irrelevant, authors assumed the diagnosis of Dercum disease.
Symptomatic treatment with analgesic, non-steroid anti-inflammatory drugs and pregabalin had an unsatisfactory response. Corticosteroids were also tried, with no better results. Use of topical lidocaine brought transitory local pain relief, but with significant recurrence. Patient was then referred for a multidisciplinary Chronic Pain consultation, with significant symptomatic improvement.
Patient was also evaluated by General Surgery and Plastic Surgery specialists, who considered that lipectomy or liposuction shouldn’t be performed at the moment, since the primary concern would be a significant weight lost. So, before any surgical intervention, patient started a demanding diet regimen and physical exercise, with a close monitoring in Nutrition consultation.
DiscussionThere are not specific management guidelines on Dercum disease’s diagnosis and treatment, since very few papers have been published on this matter.
This particular case is about a woman with the typical presentation of multiple lumps, associated with the characteristic chronic pain and obesity, the two cardinal criteria of Dercum disease. Other commonly associated disorders were also present, namely asthenia, irritability, and depressive disorder.5 In fact, in spite of the definition proposed by Hanson et al,3 other authors still consider asthenia and psychiatric disorders two diagnosis criteria, rather than associated conditions.11
Besides obesity, other cardiovascular risk factors were present, namely arterial hypertension and dyslipidaemia. Other case reports have been proposing an association between the disease and a metabolic syndrome: Szypula et al.12 described a case of a 51-year-old patient with Dercum disease who also presented severe hypercholesterolaemia and advanced atherosclerosis. Although, a causal link between the two conditions was not demonstrated. Further investigation is needed to explore the eventual role of dyslipidaemia on inflammatory response and development of fibrosis within loose connective tissue. In our case, patient presented a mild dyslipidaemia and arterial hypertension, that were reasonable controlled with medication.
Imagiology studies suggested the lipomatous nature of lesions and anatomopathological exam confirmed the presence of lipomas and fibrosis. Adipose tissue in Dercum’s disease is, in fact, characterized by the preponderance of connective tissue and fibrosis. An inflammatory infiltrate may also be present, but it is not more pronounced than that observed in healthy obese controls.3 Although biopsy is not a diagnosis criterion, it was useful to rule out other conditions such as panniculitis.
As described in this case, management of pain remains the greatest challenge in clinical approach. Pharmacological treatment is usually ineffective since disease’s pathophysiology remains unclear. Several therapeutic regimens have been described in many case reports with doubtful results,2,3,8-10 since there are not larger randomized clinical trials to support the evidence. Intravenous lidocaine has been reported to provide clinically prolonged pain relief in patients with chronic pain,13 but these findings have not been extrapolated to the specific case of Dercum disease.
Surgical approach seems to provide the most promising results in this matter. A review of literature published in 2019 evidenced significant improvement in pain, quality of life and mobility in patients who underwent liposuction, with a serious benefit in physical and psychological effects of disease.14 However, these findings are limited by retrospective evaluations with relatively short time points for measuring outcomes. Further studies are necessary, so as to assess the long-term effect of therapy as well as to define suitability criteria for liposuction. In fact, although there is a significant initial reduction of pain, this effect tends to decrease over time in many cases.15
As demonstrated, management of Dercum disease is mostly empirical, focused on pain relief and body weight reduction. As described in this particular case, the medical team has preferred a multimodal approach in order to optimize pain management and improve quality of life.
This case demonstrates the great intrinsic challenge of therapeutic management in a rare disease such as Dercum disease, since there is not validated data to rule out medical professionals’ decisions. A multidisciplinary approach with the cooperation of Internal Medicine, General and Plastic Surgery, Chronic Pain specialists and Nutrition seems to be the best option of care. The patient presented in this case will maintain a regular follow-up in those specialties, in order to lose weight, control cardiovascular risk factors, optimize pain control medication and, ultimately, perform a surgical intervention like liposuction, which still seems to be the most effective treatment.
This case report has been presented as a scientific ePoster (A-2176), with the title “Pain, pain… And no gain”, at the 17th European Congress of Internal Medicine which took place from the 30th August to 1st September, 2018, at the RheinMain CongressCenter in Wiesbaden.
Figura I

Figure 1: Nodules on dorsal region
Figura II
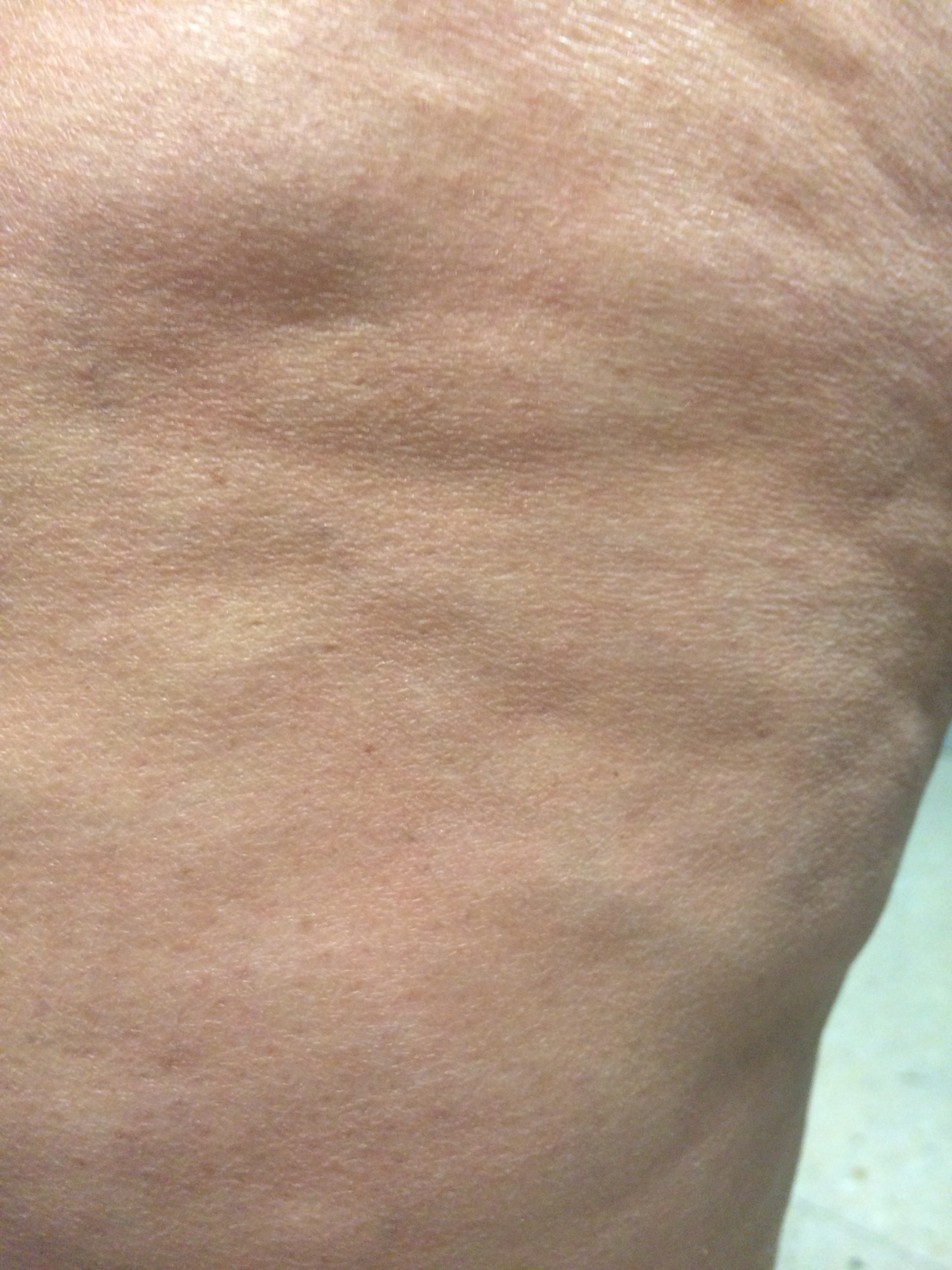
Figure 2: Nodules on dorsal region (amplified image)
Figura III

Figure 3: Nodules on inferior limbs
Figura IV

Figure 4: Ulcerative nodule on scalp
Figura V
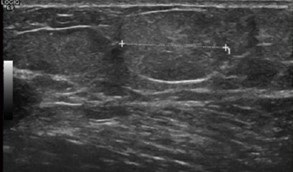
Figure 5: Ultrasound images demonstrating “echogenic lumps, with 18 and 15 mm, compatible with lipomas”
Figura VI
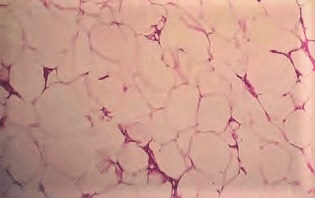
Figure 6: Anatomopathological exam, suggesting “benign neoplasm constituted by mature fatty tissue, with several lines of fibrous tissue, which characterizes a lipoma.”
BIBLIOGRAFIA
1. Herbst KL. Rare adipose disorders (RADs) masquerading as obesity. Acta Pharmacologica Sinica 2012; 33: 155–72.
2. Kucharz EJ, Kopeć-Mędrek M, Kramza J, et al. Dercum’s disease (adiposis dolorosa): a review of clinical presentation and management. Reumatologia 2019; 57, 5: 281–7 .
3. Lemaitre M, Aubert S, Chevalier B, Jannin A, Bourry J, Prévost G, et al. Rare Forms of Lipomatosis: Dercum’s Disease and Roch-Leri Mesosomatous Lipomatosis. J. Clin. Med. 2021, 10, 1292. https://doi.org/ 10.3390/jcm10061292.
4. Hansson E, Svensson H, Brorson H. Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet J Rare Dis. 2012;7:23.
5. Cook JC, Gross GP. Adiposis Dolorosa (Dercum, Anders Disease). In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 2021. [consultado 05/07/21]. Disponível em: https://www.ncbi.nlm.nih.gov/books/NBK507867/?report=printable
6. Molina JD, Nai GA, Andrade TCPC, Morgado de Abreu MAM. Dercum’s disease: a rare and underdiagnosed disease. An Bras Dermatol. 2019;94(2):251-3.
7. Herbst KL, Asare-Bediako S: Adiposis dolorosa is more than painful fat. The Endocrinologist 2007; 17:326–34.
8. Herbst KL. Subcutaneous Adipose Tissue Diseases: Dercum Disease, Lipedema, Familial Multiple Lipomatosis, and Madelung Disease. 2019. [consultado05/07/21]. Disponível em:https://www.ncbi.nlm.nih.gov/books/NBK552156/?report=printable
9.Łabuzek K, Liber S, Suchy D, Okupień B. A successful case of pain management using methformin in a patient with adiposis dolorosa. Int J Clin Pharmacol Ther 2013; 51: 517-24.
10. Eliason AH, Seo YIL, Murphy D,Beal C. Adiposis Dolorosa Pain Management. Federal Practitioner. 2019; 529-33.
11. Shaknovsky DO TJ, Salna IV DO J, Tosto Jr ST. Dercum’s Disease in A 38 Year Old White Male with Attempted Surgical Treatment: Case Report. J Dermatol Surg Res Ther 2019: 59-63.
12. Szypula I, Kotulska A, Szopa M, Pieczyrak R, Kucharz E. Adiposis dolorosa with hypercholesterolemia and premature severe generalized atherosclerosis. Wiad Lek 2009, 62:64–5.
13. Iacob E, Hagn EE, Sindt J, Brogan S, Tadler SC, Kennington KS, Hare BD, Bokat CE, Donaldson GW, Okifuji A, Junkins SR. Tertiary Care Clinical Experience with Intravenous Lidocaine Infusions for the Treatment of Chronic Pain. Pain Medicine 2018; 19: 1245–53 doi: 10.1093/pm/pnx167.
14. Williams A. A review of the literature relating to liposuction in women with lipoedema and Dercum’s disease. Journal of Lymphoedema 2019; 14 (1): 12-6.
15.Wollina U, Heinig B, Langner D, Nowak A. Juxta-articular adiposis dolorosa (Dercum disease type IV): report of four cases and treatment by dermolipectomy. Wien Med Wochenschr. 2015;165 (17-18): 374-7.