Romiplostim on refractory thrombocytopenia on systemic lupus erythematosus
Abstract
Although thrombopoetin receptor (TPOR) agonists have been approved for use in steroid-refractory primary immune thrombocytopenia (ITP), there still lacks evidence on the safety and efficacy of these drugs in patients with severe refractory thrombocytopenia associated with systemic lupus erythematosus (SLE).
We present a case of a woman with SLE for over 32 years who developed severe thrombocytopenia, refractory to multiple first-line drugs such as steroids, cyclophosphamide and rituximab and splenectomy. Although there was a good response to treatment with human intravenous immunoglobulin over several years, this drug was discontinued due to an acute coronary syndrome. She improved with romiplostim with normalization of the platelet count.
Key words: rituximab; romiplostim; systemic lupus erythematosus; thrombocytopenia
Introduction
Haematological complications are frequently seen in systemic lupus erythematosus (SLE) and may result from bone marrow failure or excessive peripheral cell destruction, both immune mediated. Thrombocytopenia (<100x109/L) is included in the American College of Rheumatology classification criteria,1 with a prevalence ranging from 7 to 30% and is among the most common clinical features of antiphospholipid syndrome (APS). Severe thrombocytopenia (platelet count < 50x109/L) occurs in 5 to 10% of patients. 2
Peripheral destruction due to autoantibodies against two platelet-specific antigens, glycoprotein IIb/IIIa and thrombopoietin receptor (TPOR), are the major pathophysiologic mechanism of thrombocytopenia in SLE. 3, 4
Many patients don’t require specific treatment for thrombocytopenia in SLE. Treatment of thrombocytopenia is usually recommended for symptomatic patients with counts less than 50x109/L and for all patients with counts bellow 20x109/L. Although treatment with steroids is often enough to control clinically significant thrombocytopenia in SLE, more intensive immunosuppression with intravenous immunoglobulin (IVIg), cyclophosphamide or rituximab may be required. These drugs are often necessary in patients relapsing upon the corticosteroids tapering (very common) and in the chronic form (typically less responsive to the steroids).
Novel treatment options for the management of cytopenias, like TPOR agonists, are promising. There are nine case reports in the literature that describe the use of romiplostim in the treatment of severe thrombocytopenia in patients with SLE.
Clinical case
We present the case of a 62 years-old, caucasian, female patient, with a diagnosis of SLE for over 32 years (six clinical – oral ulcers, joint envolvment (small articulations of the hands and wrists), leukopenia, mild thrombocytopenia, subacute cutaneous lupus and fever),and four immunologic criteria of the ACR – positive Anti-dsDNA, low C3 and C4, positive anticardiolipin antibodies and antibodies to beta-2-glycoprotein-I).
Three years after she was diagnosed she developed secondary severe thrombocytopenia (about 50 109/L) with a good initial improvement with oral corticosteroids (1mg/Kg/day). However, after 2-3 months, it relapsed upon the corticosteroids weaning. Thereafter, azathioprine (150mg/day), intravenous cyclophosphamide (750mg/month) and cyclosporine (4mg/Kg/day) were attempted, but discontinued due to leucopenia, gastrointestinal intolerance and hypertension, respectively.
After an unsuccessful danazol (600mg/day) trial, improvement was achieved with splenectomy and IVIg (0,4g/Kg/day during 5 days, every 4 weeks), followed by quarterly IVIg as maintenance treatment.
Seventeen years after the initial treatment with IVIg (April 2010), this treatment was discontinued due to a non ST elevation acute coronary syndrome during the treatment.
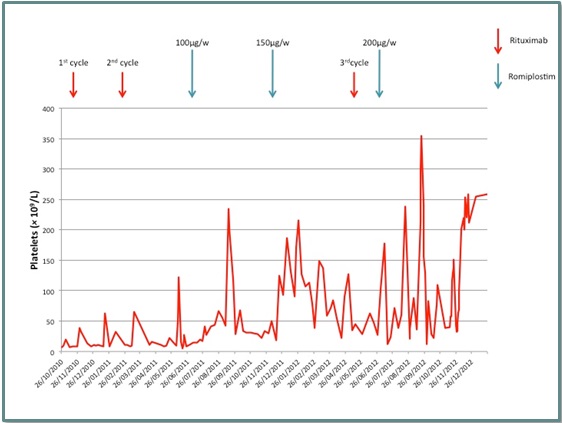
Seven months after this episode, she was started on rituximab (1g, days 1 and 15) due to recurrent and severe thrombocytopenia (5 109/L platelets). Four months later (March 2011) a second cycle was performed, but only with mild and transitory response (Fig. 1). Thus, in June 2011 romiplostim (SC injection, 1µg/Kg/week, total 50ug/week) was tried, with a stepwise dose increase to 150µg/week.
During 8 months a stable rise on platelet count to 100x109/L was obtained. Then, platelet count dropped again and an increase in steroids and a third cycle with rituximab (at May 2012) was attempted, without significant improvement.
On June 2012, severe thrombocytopenia installed again with counts around 30X109/L, having the patient multiple spontaneous ecchymosis, gum bleeding, epistaxis and bilateral subconjunctival hemorrhage. Increasing romiplostim dose to 200µg/week improved platelet count to 150-200x109/L. Therapy with romiplostim was then gradually discontinued due to frequent diarrhea and severe weight loss. After 2013 and up until 2021 the patient maintained stable platelet counts > 100x109/L.
Discussion
After several therapeutic approaches, having depleted all the pharmacological options to control the refractory thrombocytopenia, the off-label use of romiplostim was a powerful weapon on aiding the control of platelet counts.
Romiplostim is a thrombopoetin receptor (TPOR) agonist that stimulates megakaryopoiesis. It is approved for the treatment of chronic refractory primary immune thrombocytopenic purpura (ITP), improving quality of life in these patients. It is a well-tolerated drug, being headache, myalgia, arthralgia, nausea and diarrhea the most frequent side effects. The duration of treatment with TPOR can be indefinite if well tolerated but 20-30% of patients can maintain stable counts despite reduction and suspension of therapy. According to the most recent guidelines in patients with stable platelet counts (50-100x109/L for over 6 months or >100x109/L for over 3 months) a gradual reduction (3 to 12 months) and ultimately suspension of therapy with TPOR is recommended.5
The presence of antibodies against the TPOR, mainly associated with antiphospholipid syndrome (APS), may be associated with a poorer response to steroids and IVIg 4.
In the literature review we found nine case reports of patients with SLE-associated ITP refractory to treatment with steroids and other immunosuppressive therapy treated with romiplostim. The first case report6 showed the efficacy of romiplostim in the treatment of severe thrombocytopenia associated to Evans syndrome refractory to rituximab and the second case7 described a successful treatment with romiplostim of a pregnant woman with SLE and severe thrombocytopenia, which was resistant to several treatment options, including steroids, IVIg and Rituximab. In both cases the drug was well-tolerated and there were no significant adverse events.
In the third report,8 a retrospective study in Danish haematology departments, the use of a TPOR in thrombocytopenia secondary to SLE in one patient was discontinued due to lack of effect.
The fourth case9 presented a 19-year-old female with the diagnosis of thrombocytopenia secondary to SLE and refractory to treatment with steroids, rituximab and IVIg. Kidney-limited thrombotic microangiopathy following treatment with romiplostim is a possibility that explained the acute renal failure developed in this patient after the initiation of the TPOR (romiplostim acted as a trigger in a predisposed patient), although the incidence of thrombotic events was not different between the patients with chronic ITP treated with romiplostim compared with placebo.10
In the fifth case, a 39-year-old woman with immune thrombocytopenia associated with SLE refractory to high dose of corticosteroids, IVIG and rituximab, had a great improvement, with complete response, with romiplostim.11
The last four reports are from a case series published in 2018.12 They report a case of a 45-year-old woman with class IV/V lupus nephritis, pericarditis, malar rash and thrombocytopenia. Her therapy initially included high dose steroids, hydroxychloroquine (later stopped due to concern of eye disease) and mycophenolate mofetil. Due to recurrent pericarditis and tamponade, she required a pericardial window. The post-op period was complicated due to persistent chest wall bleeding due to severe thrombocytopenia (16X109/L). She was started on romiplostim 1mcg/Kg/week, later increased to 2mcg/Kg after the first week. Although platelet count increased (peak of 368x109/L one month after starting romiplostim), the patient died shortly after due to septic shock.
The second case report of the case series is about a 58-year-old woman with thrombocytopenia associated with SLE refractory to high dose of corticosteroids, IVIG and rituximab, who had a favorable response to therapy with romiplostim, which she continued for three years, later switching to eltrombopag due to insurance concerns. The patient was lost to follow up.
The third case of the case series is about a female 55-year-old patient patient with LES and thrombocytopenia who presented for a foot surgery with a platelet count of 40-50x109/L. She did not respond to platelet transfusions nor to IVIg therapy. Surgery was postponed and the patient was started on romiplostim 1mcg/Kg/week, and three weeks later on 2mcg/Kg/week. After one week of this dose the patient had a platelet count of 99x109/L and underwent foot surgery. After the patient was lost to follow up.
The last case is one of a 23-year-old female LES patient with thrombocytopenia (50-120x109/L) and severe APS with multiple embolic complications (deep vein thrombosis, pulmonary embolism, acute coronary syndrome) despite trials on several anticoagulants. She was admitted for gastrointestinal bleeding due to ischemic colitis. At the time she mas on methylprednisolone 48mg/day; monthly IVIg over the prior 2 months and one dose of belimumab in the prior month. Shortly after admission she developed diffuse alveolar hemorrhage and received stress-dose corticosteroids and plasmapheresis. Two weeks later her thrombocytopenia worsened to 20x109/L. She underwent therapy with IVIg with short term response and then was started on weekly romiplostim given the need for lifelong anticoagulation. Her platelet count improved to 64x109/L but after leveled in the range of 10-40x109/L. She died shortly after.
To conclude the authors would like to highlight that although the management of thrombocytopenia can be challenging, novel therapeutic approaches including TPOR agonists are promising, and more prospective controlled research is needed in this field.
Figura I
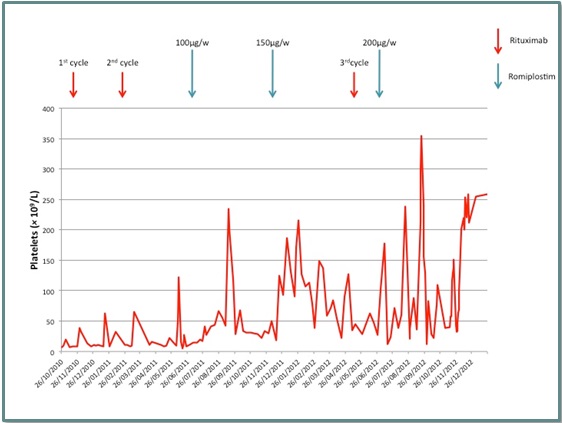
Platelet levels evolution throughout time according to rituximab and romiplostim treatments.
BIBLIOGRAFIA
1. Petri M, Orbai AM, Alarcón GS, et al. Derivation and validation of systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 2012; 64: 2677-2686;
2. Wallace DJ. The clinical presentation of systemic lupus erythematosus. In: Wallace DJ, Han BH (eds), Dubois´ lupus erythematosus. Baltimore, MD: Williams & Wilkins, 1997. p 638-646;
3. Ziakas PO, Routsias JG, Giannouli S, Tasidou A, Tizioufas AG, Voulgarelis M. Suspects in the tale of lupus-associated thrombocytopenia. Clin Exp Immunol 2006; 145: 71-80;
4. Kuwana M, Kaburaki J, Okazaki Y, Miyazaki H, Ikeda Y, Two types of autoantibody-mediated thrombocytopenia in patients with systemic lupus erythematosus. Rheumatology 2006; 45: 851-854;
5. Lozano ML, Sanz MA, Vicente V. Recomendaciones del Grupo Español de PTI para el diagnostico, tratamento y seguimento de pacientes con trombocytopenia inmune. Med Clin 2021;
6. Gonzalez-Nieto JA, Martin-Suarez I, Quattrino S, Ortiz-Lopez E, Munoz-Beamud FR, Colchero-Fernandez J,et al. The efficacy of romiplostim in the treatment of severe thrombocytopenia associated to Evans syndrome refractory to rituximab. Lupus 2011; 20: 1321-1323;
7. Alkaabi JK, Alkindi S, Riyami NA, Zia F, Balla LM, Balla SM. Successful treatment of severe thrombocytopenia with romiplostim in a pregnant patient with systemic lupus erythematosus. Lupus 2012; 21: 1571-1574;
8. Gudbrandsdottir S, Frederiksen H, Hasselbalch H. Thrombopoietin-receptor agonists in haematological disorders: the Danish experience. Platelets 2012; 23: 423-429;
9. Tomov S, Lazarchick J, Self SE, Bruner ET, Budisavljevic MN. Kidney-limited thrombotic microangiopathy in patients with SLE treated with romiplostim. Lupus 2013; 22: 504-509;
10. Gernsheimer TB, George JN, Aledort LM, Tarantino MD, Sunkara U, Matthew Guo D, et al. Evaluation of bleeding and thrombotic events during long-term use of romiplostim in patients with chronic immune thrombocytopenia (ITP). J Thromb Haemost 2010; 8: 1372-1382;
11. Magnano L, Enríquez H, Esteve J, Cervera R and Espinosa G. Effectiveness of thrombopoietin-receptor agonists in the treatment of refractory imune thrombocytopenia associated to systemic lupus erythematosus. J Rheumatol 2014; 41 (9): 1895-1896;
12. Lusa A, Carlson A. Safety and efficacy of thrombopoeitin mimetics for refractory immune thrombocytopenia purpura in patients with systemic lupus erythematosus or antiphospholipid syndrome: a case series. Lupus. 2018 Sep;27(10):1723-1728.